5 Mind-Blowing Facts About Stress and Chronic Visceral Pain
Discover 5 mind-blowing facts that reveal the intricate link between stress and chronic visceral pain. Learn how to protect your gut health now!
Key Points
- Visceral pain and stress are interconnected, affecting the gut-brain axis and influencing the body's response to environmental challenges.
- Chronic visceral pain and stress can become independent health issues, prevalent in disorders of gut-brain interaction (DGBI).
- Women are more likely to suffer from chronic visceral pain, with sex hormones, stress, and its correlates playing a significant role.
- Research is needed to understand the interactions between altered visceroception, stress, and sex, especially in clinical populations with DGBI.
- A lifespan perspective in future research could provide valuable insights for tailored prevention strategies and therapeutic approaches for chronic visceral pain and DGBI.
Pain and Stress in Gut-Brain Interaction Disorders
The intertwining of pain and stress is a complex phenomenon, that affects our body's balance and health regulation A Trusted Source Timmers, I, Quaedflieg, CWEM, Hsu, C, Heathcote, LC, Rovnaghi, CR, and Simons, LE. The interaction between stress and chronic pain through the lens of threat learning.Neurosci Biobehav Rev. (2019) 107:641–55. doi: 10.1016/j.neubiorev.2019.10.007 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Panerai, AE. Pain emotion and homeostasis.Neurol Sci. (2011) 32:27–9. doi: 10.1007/s10072-011-0540-5 CrossRef Full TextGoogle Scholar A Trusted Source Schulz, A, and Vögele, C. Interoception and stress.Front Psychol. (2015) 6:993. doi: 10.3389/fpsyg.2015.00993 PubMed AbstractCrossRef Full TextGoogle Scholar .
Pain and stress can sometimes outlive their initial cause, becoming independent health problems and significantly affecting quality of life.

How Stress Influences Chronic Visceral Pain Disorders
Research has particularly highlighted the role of stress in gut-brain interaction disorders like irritable bowel syndrome (IBS), which affects up to 10% of the global population A Trusted Source 4. Ford, AC, Sperber, AD, Corsetti, M, and Camilleri, M. Irritable bowel syndrome.Lancet. (2020) 396:1675–88. doi: 10.1016/S0140-6736(20)31548-8 CrossRef Full TextGoogle Scholar .
Stress can exacerbate pain sensitivity, affect gut movement, and alter brain responses to pain in IBS patients A Trusted Source Schaper, SJ, and Stengel, A. Emotional stress responsivity of patients with IBS—a systematic review.J Psychosom Res. (2022) 153:110694. doi: 10.1016/j.jpsychores.2021.110694 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Elsenbruch, S, Rosenberger, C, Bingel, U, Forsting, M, Schedlowski, M, and Gizewski, ER. Patients with irritable bowel syndrome have altered emotional modulation of neural responses to visceral stimuli.Gastroenterology. (2010) 139:1310–1319.e4. doi: 10.1053/j.gastro.2010.06.054 PubMed AbstractCrossRef Full TextGoogle Scholar .
Prolonged stress can lead to dysregulated systems in the body, which can negatively impact gut-brain communication A Trusted Source Enck, P, Aziz, Q, Barbara, G, Farmer, AD, Fukudo, S, Mayer, EA, et al. Irritable bowel syndrome.Nat Rev Dis Primers. (2016) 2:16014. doi: 10.1038/nrdp.2016.14 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Woda, A, Picard, P, and Dutheil, F. Dysfunctional stress responses in chronic pain.Psychoneuroendocrinology. (2016) 71:127–35. doi: 10.1016/j.psyneuen.2016.05.017 CrossRef Full TextGoogle Scholar .
This makes IBS a condition deeply related to stress.
Women and the Predominance of Pain and Stress Disorders
Interestingly, women are more prone to develop conditions characterized by pain and stress A Trusted Source Fillingim, RB, King, CD, Ribeiro-Dasilva, MC, Rahim-Williams, B, and Riley, JL. Sex, gender, and pain: a review of recent clinical and experimental findings.J Pain. (2009) 10:447–85. doi: 10.1016/j.jpain.2008.12.001PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Swaab, DF, and Bao, A-M. Sex differences in stress-related disorders: major depressive disorder, bipolar disorder, and posttraumatic stress disorder.Handb Clin Neurol. (2020) 175:335–58. doi: 10.1016/B978-0-444-64123-6.00023-0 PubMed AbstractCrossRef Full TextGoogle Scholar .
Pronounced sex differences are evident in gut-brain interaction disorders, with stress playing a significant role in these differences A Trusted Source Lovell, RM, and Ford, AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis.Clin Gastroenterol Hepatol. (2012) 10:712–721.e4. doi: 10.1016/j.cgh.2012.02.029 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Labanski, A, Langhorst, J, Engler, H, and Elsenbruch, S. Stress and the brain-gut axis in functional and chronic-inflammatory gastrointestinal diseases: a transdisciplinary challenge.Psychoneuroendocrinology. (2020) 111:104501. doi: 10.1016/j.psyneuen.2019.104501PubMed AbstractCrossRef Full TextGoogle Scholar .
However, it's important to note that while data supports these observations, experimental studies have shown variability,
with no clear conclusion that women are necessarily more sensitive to stress or pain A Trusted Source Racine, M, Tousignant-Laflamme, Y, Kloda, LA, Dion, D, Dupuis, G, and Choinière, M. A systematic literature review of 10 years of research on sex/gender and experimental pain perception—part 1: are there really differences between women and men?Pain. (2012) 153:602–18. doi: 10.1016/j.pain.2011.11.025 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Greenspan, JD, Craft, RM, LeResche, L, Arendt-Nielsen, L, Berkley, KJ, Fillingim, RB, et al. Studying sex and gender differences in pain and analgesia: a consensus report.Pain. (2007) 132:S26–45. doi: 10.1016/j.pain.2007.10.014 PubMed AbstractCrossRef Full TextGoogle Scholar .
Interaction Between Pain, Stress, and Sex in Gut-Brain Disorders
This article will delve into the role of stress in gut-brain disorders, emphasizing the influence of sex on this interaction.
Research on the neurobiology of stress and its effects on gut-brain communication is essential to understanding these complexities.
Unlocking the Secrets of the Gut-Brain Connection
Our guts and brains are in constant communication, a complex dance affecting everything from our pain levels to our stress responses A Trusted Source Black, CJ, Drossman, DA, Talley, NJ, Ruddy, J, and Ford, AC. Functional gastrointestinal disorders: advances in understanding and management.Lancet. (2020) 396:1664–74. doi: 10.1016/S0140-6736(20)32115-2 CrossRef Full TextGoogle Scholar .
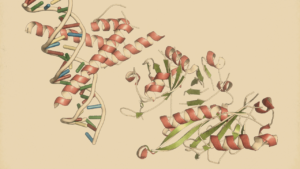
This "gut-brain axis" is a fascinating, multi-directional pathway involving bio-psychosocial modulators A Trusted Source Carabotti, M, Scirocco, A, Maselli, MA, and Severi, C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems.Ann Gastroenterol. (2015) 28:203–9.http://www.ncbi.nlm.nih.gov/pubmed/25830558. PubMed AbstractGoogle Scholar .
The Players in Our Gut-Brain Communication
At the heart of the gut-brain axis are the enteric nervous system (ENS) and the central nervous system (CNS), connecting through a network of pathways to keep our body in balance A Trusted Source Margolis, KG, Gershon, MD, and Bogunovic, M. Cellular organization of neuroimmune interactions in the gastrointestinal tract.Trends Immunol. (2016) 37:487–501. doi: 10.1016/j.it.2016.05.00 3PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Rao, M, and Gershon, MD. The bowel and beyond: the enteric nervous system in neurological disorders.Nat Rev Gastroenterol Hepatol. (2016) 13:517–28. doi: 10.1038/nrgastro.2016.107 PubMed AbstractCrossRef Full TextGoogle Scholar .
Our brains, along with various other systems, modulate gut function.
Psychological factors also play a role, in affecting our responses to visceral sensations A Trusted Source Menon, V.Salience network. Elsevier Inc. (2015). 597–611 Google Scholar A Trusted Source Mayer, EA, Gupta, A, Kilpatrick, LA, and Hong, J-Y. Imaging brain mechanisms in chronic visceral pain.Pain. (2015) 156:S50–63. doi: 10.1097/j.pain.0000000000000106 CrossRef Full TextGoogle Scholar A Trusted Source Borsook, D, Edwards, R, Elman, I, Becerra, L, and Levine, J. Pain and analgesia: the value of salience circuits.Prog Neurobiol. (2013) 104:93–105. doi: 10.1016/j.pneurobio.2013.02.003 PubMed AbstractCrossRef Full TextGoogle Scholar .
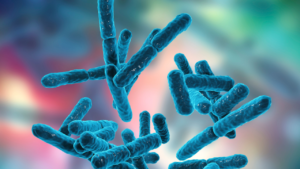
Stress: A Major Player in Gut Health
Stress can have profound effects on our gut health, influencing the microbial composition and potentially playing a role in chronic visceral pain A Trusted Source Margolis, KG, Cryan, JF, and Mayer, EA. The microbiota-gut-brain axis: from motility to mood.Gastroenterology. (2021) 160:1486–501. doi: 10.1053/j.gastro.2020.10.066 PubMed AbstractCrossRef Full TextGoogle Scholar .
Stress impacts gut motility and can lead to alterations in gut permeability and visceral hyperalgesia A Trusted Source Taché, Y, and Million, M. Role of corticotropin-releasing factor signaling in stress-related alterations of colonic motility and hyperalgesia.J Neurogastroenterol Motil. (2015) 21:8–24. doi: 10.5056/jnm14162 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Overman, EL, Rivier, JE, and Moeser, AJ. CRF induces intestinal epithelial barrier injury via the release of mast cell proteases and TNF-α.PLoS One. (2012) 7:e39935. doi: 10.1371/journal.pone.0039935 PubMed AbstractCrossRef Full TextGoogle Scholar .
The Impact of Stress on Our Guts: A Closer Look
Studies have shown that stress can alter gut permeability, even in healthy individuals A Trusted Source Vanuytsel, T, van Wanrooy, S, Vanheel, H, Vanormelingen, C, Verschueren, S, Houben, E, et al. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism.Gut. (2014) 63:1293–9. doi: 10.1136/gutjnl-2013-305690 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Gerdin, L, González-Castro, AM, Ericson, A-C, Persborn, M, Santos, J, Walter, SA, et al. Acute psychological stress increases paracellular permeability and modulates immune activity in rectal mucosa of healthy volunteers.United European Gastroenterol J. (2023) 11:31–41. doi: 10.1002/ueg2.12329 PubMed AbstractCrossRef Full TextGoogle Scholar .
It also affects our mood, cognition, and brain function A Trusted Source Roderigo, T, Benson, S, Schöls, M, Hetkamp, M, Schedlowski, M, Enck, P, et al. Effects of acute psychological stress on placebo and nocebo responses in a clinically relevant model of visceroception.Pain. (2017) 158:1489–98. doi: 10.1097/j.pain.0000000000000940 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Rosenberger, C, Elsenbruch, S, Scholle, A, De Greiff, A, Schedlowski, M, Forsting, M, et al. Effects of psychological stress on the cerebral processing of visceral stimuli in healthy women.Neurogastroenterol Motil. (2009) 21:740–e45. doi: 10.1111/j.1365-2982.2009.01295.x PubMed AbstractCrossRef Full TextGoogle Scholar .
When a study introduced an experimental visceral pain model, they saw that stress also affects visceral perception, particularly in women A Trusted Source Kano, M, Muratsubaki, T, Van Oudenhove, L, Morishita, J, Yoshizawa, M, Kohno, K, et al. Altered brain and gut responses to corticotropin-releasing hormone (CRH) in patients with irritable bowel syndrome.Sci Rep. (2017) 7:12425. doi: 10.1038/s41598-017-09635-x PubMed AbstractCrossRef Full TextGoogle Scholar .
These findings underscore the importance of further research to fully understand the intricate relationship between stress, sex, and our gut-brain axis.
Stress and its Impact on Our Bodies and Minds
Stress triggers an intricate response from our body and mind, launching a symphony of reactions that help us face challenges or prepare for potential stressors A Trusted Source McEwen, BS, and Akil, H. Revisiting the stress concept: implications for affective disorders.J Neurosci. (2020) 40:12–21. doi: 10.1523/JNEUROSCI.0733-19.2019 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Sanacora, G, Yan, Z, and Popoli, M. The stressed synapse 2.0: pathophysiological mechanisms in stress-related neuropsychiatric disorders.Nat Rev Neurosci. (2022) 23:86–103. doi: 10.1038/s41583-021-00540-x PubMed AbstractCrossRef Full TextGoogle Scholar .
However, when stress becomes chronic, it can transform from a helpful ally to a formidable foe, setting the stage for mental and somatic disorders, including chronic pain A Trusted Source Crofford, LJ. Chronic pain: where the body meets the brain.Trans Am Clin Climatol Assoc. (2015) 126:167–83. Available at:https://pubmed.ncbi.nlm.nih.gov/26330672/ Google Scholar .
The Inner Workings of Our Stress Response
Two main actors govern our body’s response to stress.
The first is the activation of the sympathetic nervous system, resulting in the release of (nor)epinephrine, which elevates our heart rate and blood pressure A Trusted Source McEwen, BS. Stress, adaptation, and disease. Allostasis and allostatic load.Ann N Y Acad Sci. (1998) 840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x CrossRef Full TextGoogle Scholar .
The second actor is the hypothalamus-pituitary-adrenocortical (HPA) axis, which releases corticotropin-releasing hormone (CRH) from the hypothalamus.
This chain reaction leads to the secretion of adrenocorticotropic hormone into our bloodstream, ultimately releasing cortisol from the adrenal cortex.
This hormone has far-reaching effects, interacting with various brain regions, including the amygdala, hippocampus, and prefrontal cortex A Trusted Source. Joëls, M, and Baram, TZ. The neuro-symphony of stress.Nat Rev Neurosci. (2009) 10:459–66. doi: 10.1038/nrn2632 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Rodrigues, SM, LeDoux, JE, and Sapolsky, RM. The influence of stress hormones on fear circuitry.Annu Rev Neurosci. (2009) 32:289–313. doi: 10.1146/annurev.neuro.051508.135620 PubMed AbstractCrossRef Full TextGoogle Scholar .
The Intriguing Dance of Stress, Sex, and Hormones
Stress responses are not a one-size-fits-all phenomenon; they differ between men and women and hinge on the availability of sex hormones A Trusted Source Kudielka, BM, and Kirschbaum, C. Sex differences in HPA axis responses to stress: a review.Biol Psychol. (2005) 69:113–32. doi: 10.1016/j.biopsycho.2004.11.009 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Taylor, SE, Klein, LC, Lewis, BP, Gruenewald, TL, Gurung, RA, and Updegraff, JA. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight.Psychol Rev. (2000) 107:411–29. doi: 10.1037/0033-295x.107.3.411 CrossRef Full TextGoogle Scholar .
For instance, during the follicular phase of the menstrual cycle, when female sex hormone concentrations are low, cortisol release is reduced compared to the luteal phase, which is marked by higher levels of estradiol and progesterone A Trusted Source Kajantie, E, and Phillips, DIW. The effects of sex and hormonal status on the physiological response to acute psychosocial stress.Psychoneuroendocrinology. (2006) 31:151–78. doi: 10.1016/j.psyneuen.2005.07.002PubMed AbstractCrossRef Full TextGoogle Scholar .
Similarly, the intake of hormonal contraceptives, which lower endogenous sex hormone availability, can also diminish or even blunt cortisol release in response to acute stress A Trusted Source Gervasio, J, Zheng, S, Skrotzki, C, and Pachete, A. The effect of oral contraceptive use on cortisol reactivity to the Trier social stress test: a meta-analysis.Psychoneuroendocrinology. (2022) 136:105626. doi: 10.1016/j.psyneuen.2021.105626 PubMed AbstractCrossRef Full TextGoogle Scholar .
These interactions between stress and female sex hormones play a pivotal role in various processes, such as memory, fear conditioning, and emotion regulation,
which are all crucial in the context of pain and its modulation A Trusted Source Meulders, A. Fear in the context of pain: lessons learned from 100 years of fear conditioning research.Behav Res Ther. (2020) 131:103635. doi: 10.1016/j.brat.2020.103635 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Elsenbruch, S, Benson, S, Koenen, LR, Labrenz, F, and Icenhour, A. From gut feelings to memories of visceral pain.Neuroforum. (2020) 26:171–7. doi: 10.1515/nf-2020-0016 CrossRef Full TextGoogle Scholar .
Testosterone, an androgen, also plays a part in this complex dance, partially mediated by its conversion to estradiol A Trusted Source Zuloaga, DG, Heck, AL, De Guzman, RM, and Handa, RJ. Roles for androgens in mediating the sex differences of neuroendocrine and behavioral stress responses.Biol Sex Differ. (2020) 11:44. doi: 10.1186/s13293-020-00319-2 PubMed AbstractCrossRef Full TextGoogle Scholar .
While rodent models hint at a protective role of testosterone in pain contexts A Trusted Source Aloisi, AM. Gonadal hormones and sex differences in pain reactivity.Clin J Pain. (2003) 19:168–74. doi: 10.1097/00002508-200305000-00004 PubMed AbstractCrossRef Full TextGoogle Scholar, including visceral pain A Trusted Source Ji, Y, Hu, B, Li, J, and Traub, RJ. Opposing roles of estradiol and testosterone on stress-induced visceral hypersensitivity in rats.J Pain. (2018) 19:764–76. doi: 10.1016/j.jpain.2018.02.007 PubMed AbstractCrossRef Full TextGoogle Scholar ,
human research is still catching up, and findings are somewhat mixed A Trusted Source Archey, M, Goldey, K, Crockett, E, and Boyette-Davis, J. An investigation of the effects of testosterone and behavioral expressions of pain on sex/gender differences in pain perception.Psychol Rep. (2019) 122:826–40. doi: 10.1177/0033294118781320 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Racine, M, Tousignant-Laflamme, Y, Kloda, LA, Dion, D, Dupuis, G, and Choinière, M. A systematic literature review of 10 years of research on sex/gender and pain perception—part 2: do biopsychosocial factors alter pain sensitivity differently in women and men?Pain. (2012) 153:619–35. doi: 10.1016/j.pain.2011.11.026 PubMed AbstractCrossRef Full TextGoogle Scholar .
A Need for Further Exploration
The interconnectedness of pain, stress, and sex is a widely discussed topic, crucial for understanding the vast interindividual variability in pain and stress-related disorders A Trusted Source Slavich, GM, and Sacher, J. Stress, sex hormones, inflammation, and major depressive disorder: extending social signal transduction theory of depression to account for sex differences in mood disorders.Psychopharmacology. (2019) 236:3063–79. doi: 10.1007/s00213-019-05326-9 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Martínez-Lavín, M. Fibromyalgia in women: somatisation or stress-evoked, sex-dimorphic neuropathic pain?Clin Exp Rheumatol. (2021) 39:422–5. doi: 10.55563/clinexprheumatol/0c7d6v PubMed AbstractCrossRef Full TextGoogle Scholar ,
including disorders like DGBI A Trusted Source Van Oudenhove, L, Crowell, MD, Drossman, DA, Halpert, AD, Keefer, L, Lackner, JM, et al. Biopsychosocial aspects of functional gastrointestinal disorders.Gastroenterology. (2016) S0016–5085(16)00218-3. doi: 10.1053/j.gastro.2016.02.027 PubMed AbstractCrossRef Full TextGoogle Scholar .
However, the specific processes and mechanisms underlying these interactions remain elusive, calling for further research to fully uncover the intricacies of this fascinating triad.
Dance of Sex, Stress, and Pain in Gut-Brain Communication: A Lifespan Perspective
When considering disorders of gut-brain interaction (DGBI), stress and female sex have been consistently flagged as significant risk factors A Trusted Source Black, CJ, and Ford, AC. Global burden of irritable bowel syndrome: trends, predictions and risk factors.Nat Rev Gastroenterol Hepatol. (2020) 17:473–86. doi: 10.1038/s41575-020-0286-8 PubMed AbstractCrossRef Full TextGoogle Scholar .
Notably, sex differences have been observed in prevalence, pathophysiological factors, clinical characteristics, and responses to therapy A Trusted Source Narayanan, SP, Anderson, B, and Bharucha, AE. Sex- and gender-related differences in common functional gastroenterologic disorders.Mayo Clin Proc. (2021) 96:1071–89. doi: 10.1016/j.mayocp.2020.10.004PubMed AbstractCrossRef Full TextGoogle Scholar .
A Biopsychosocial Approach to Understand the Intricacies
A multidimensional perspective - the supersystems approach - has recently been employed to elucidate the connections between pain and stress,
incorporating reciprocal neural, endocrine, and immune interactions A Trusted Source Chapman, CR, Tuckett, RP, and Song, CW. Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions.J Pain. (2008) 9:122–45. doi: 10.1016/j.jpain.2007.09.006PubMed AbstractCrossRef Full TextGoogle Scholar .
This framework has evolved to include dysregulations that underpin sexually dimorphic effects within a biopsychosocial model A Trusted Source Bartley, EJ, and Fillingim, RB. Chapter 4—sex differences in pain and stress In: M Al’absi and MA Flaten, editors.Neuroscience of pain, stress, and emotion. San Diego: Academic Press (2016). 77–95.Google Scholar .
Various factors, such as central nervous system processing, genetic factors, and the responsivity of the hypothalamus-pituitary-adrenocortical (HPA) and sympatho-medullary axes,
are entwined with sex hormones and their fluctuations across the menstrual cycle, playing a significant role in visceral pain and DGBI.
However, these factors interact with psychosocial elements ranging from predispositions to anxiety and depression to gender roles and cultural influences,
heightening women’s vulnerability to chronic visceral pain A Trusted Source Black, CJ, Drossman, DA, Talley, NJ, Ruddy, J, and Ford, AC. Functional gastrointestinal disorders: advances in understanding and management.Lancet. (2020) 396:1664–74. doi: 10.1016/S0140-6736(20)32115-2 CrossRef Full TextGoogle Scholar .
The Crucial Element: Age-Related Effects
A pivotal aspect that is gaining increasing attention in animal models but has been relatively overlooked in humans is the impact of aging on the interplay between visceral pain, stress, and sex-related effects A Trusted Source Hodes, GE, and Epperson, CN. Sex differences in vulnerability and resilience to stress across the life span.Biol Psychiatry. (2019) 86:421–32. doi: 10.1016/j.biopsych.2019.04.028 PubMed AbstractCrossRef Full TextGoogle Scholar .
Age-related changes can directly influence sex hormone concentrations or HPA axis activity, and indirectly bring about secondary changes through environmental and lifestyle factors A Trusted Source Gupta, D, and Morley, JE. Hypothalamic-pituitary-adrenal (HPA) axis and aging.Compr Physiol. (2014) 4:1495–510. doi: 10.1002/cphy.c130049 CrossRef Full TextGoogle Scholar A Trusted Source Chahal, HS, and Drake, WM. The endocrine system and ageing.J Pathol. (2007) 211:173–80. doi: 10.1002/path.2110 CrossRef Full TextGoogle Scholar .
Sensitive Periods of Life: Windows of Vulnerability
Stressors during sensitive life stages can have lasting effects.
For instance, psychosocial adversity pre- or postnatally can cause profound detrimental impacts on offspring, with manifestations potentially occurring later in life A Trusted Source Murgatroyd, C, Patchev, AV, Wu, Y, Micale, V, Bockmühl, Y, Fischer, D, et al. Dynamic DNA methylation programs persistent adverse effects of early-life stress.Nat Neurosci. (2009) 12:1559–66. doi: 10.1038/nn.2436 PubMed AbstractCrossRef Full TextGoogle Scholar .
Such manifestations often differ between sexes, with females exhibiting passive coping and symptoms of anxiety and depression, known risk factors for stress-related disorders like DGBI A Trusted Source Chaloner, A, and Greenwood-Van Meerveld, B. Early life adversity as a risk factor for visceral pain in later life: importance of sex differences.Front Neurosci. (2013) 7:13. doi: 10.3389/fnins.2013.00013PubMed AbstractCrossRef Full TextGoogle Scholar .
Critical Developmental Phases: Puberty and Menopause
Puberty, a period marked by hormonal changes and sexual maturation, interacts with the gut’s microbiome, affecting its composition in a sex-specific manner A Trusted Source Korpela, K, Kallio, S, Salonen, A, Hero, M, Kukkonen, AK, Miettinen, PJ, et al. Gut microbiota develop towards an adult profile in a sex-specific manner during puberty.Sci Rep. (2021) 11:23297. doi: 10.1038/s41598-021-02375-z PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Calcaterra, V, Rossi, V, Massini, G, Regalbuto, C, Hruby, C, Panelli, S, et al. Precocious puberty and microbiota: the role of the sex hormone-gut microbiome axis.Front Endocrinol. (2022) 13:1000919. doi: 10.3389/fendo.2022.1000919 PubMed AbstractCrossRef Full TextGoogle Scholar .
Stress can interfere with gut microbiota, contributing to gut dysbiosis in a sex-specific manner A Trusted Source Tsilimigras, MCB, Gharaibeh, RZ, Sioda, M, Gray, L, Fodor, AA, and Lyte, M. Interactions between stress and sex in microbial responses within the microbiota-gut-brain axis in a mouse model.Psychosom Med. (2018) 80:361–9. doi: 10.1097/PSY.0000000000000572 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Esposito, P, and Ismail, N. Linking puberty and the gut microbiome to the pathogenesis of neurodegenerative disorders.Microorganisms. (2022) 10:2163. doi: 10.3390/microorganisms10112163 PubMed AbstractCrossRef Full TextGoogle Scholar .
Consequently, stressors during puberty can significantly affect the vulnerability to dysregulated gut-brain communication.
Conversely, post-menopause, a decline in ovarian hormone concentrations correlates with a decreased incidence of DGBI in women A Trusted Source Cain, KC, Jarrett, ME, Burr, RL, Rosen, S, Hertig, VL, and Heitkemper, MM. Gender differences in gastrointestinal, psychological, and somatic symptoms in irritable bowel syndrome.Dig Dis Sci. (2009) 54:1542–9. doi: 10.1007/s10620-008-0516-3 PubMed AbstractCrossRef Full TextGoogle Scholar .
However, this trend may reverse in women undergoing hormone replacement therapy A Trusted Source Ruigómez, A, García Rodríguez, LA, Johansson, S, and Wallander, M-A. Is hormone replacement therapy associated with an increased risk of irritable bowel syndrome?Maturitas. (2003) 44:133–40. doi: 10.1016/s0378-5122(02)00321-3 PubMed AbstractCrossRef Full TextGoogle Scholar .
A Call for Future Research
While the age-related effects and their interplay with sex and stress are well-established, there's a need for further research,
particularly considering lifespan-related phenomena when investigating complex sex-stress-pain interactions in both healthy individuals and patients with DGBI A Trusted Source Gaffey, AE, Bergeman, CS, Clark, LA, and Wirth, MM. Aging and the HPA axis: stress and resilience in older adults.Neurosci Biobehav Rev. (2016) 68:928–45. doi: 10.1016/j.neubiorev.2016.05.036 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Soenen, S, Rayner, CK, Jones, KL, and Horowitz, M. The ageing gastrointestinal tract.Curr Opin Clin Nutr Metab Care. (2016) 19:12–8. doi: 10.1097/MCO.0000000000000238 CrossRef Full TextGoogle Scholar .

Challenges and Future Directions
The variation in individual experiences and treatments of clinical visceral pain in disorders of gut-brain interaction (DGBI) presents a substantial healthcare challenge A Trusted Source Camilleri, M. Diagnosis and treatment of irritable bowel syndrome: a review.JAMA. (2021) 325:865–77. doi: 10.1001/jama.2020.22532 CrossRef Full TextGoogle Scholar .
The optimal approach for comprehending this intricate web of influences on pain experiences and risk of chronification is through a biopsychosocial disease model A Trusted Source Fillingim, RB. Individual differences in pain: understanding the mosaic that makes pain personal.Pain. (2017) 158:S11–8. doi: 10.1097/j.pain.0000000000000775 PubMed AbstractCrossRef Full TextGoogle Scholar .
This model proposes that research and translational approaches should consider central, neuroendocrine, immunological, and enteric mechanisms, alongside the effects of stress, hormonal fluctuations, and psychosocial factors, to wholly appreciate complex chronic pain conditions.
Incorporating a lifespan perspective, focusing on long-term studies and especially vulnerable life periods, is a promising future direction for comprehensive understanding and personalized treatment options A Trusted Source Campisi, J, Kapahi, P, Lithgow, GJ, Melov, S, Newman, JC, and Verdin, E. From discoveries in ageing research to therapeutics for healthy ageing.Nature. (2019) 571:183–92. doi: 10.1038/s41586-019-1365-2 PubMed AbstractCrossRef Full TextGoogle Scholar .
Discussion
- Exploration of the complex relationship between chronic visceral pain and stress.
- The significant role of stress in exacerbating pain sensitivity and affecting gut movement and brain responses in patients with gut-brain interaction disorders.
- Analysis of pronounced sex differences in the prevalence and characteristics of pain and stress disorders, with women being more prone to these conditions.
- The a need for further research to fully understand the intricacies of the gut-brain axis and the interconnectedness of pain, stress, and sex.
Conclusion
- The article highlights the vital role of stress in gut-brain interaction disorders, particularly in women.
- It underscores the importance of a comprehensive approach to understanding the complexities of the gut-brain axis, incorporating biopsychosocial models and lifespan perspectives.
- The findings of the article stress the need for more research to unravel the specific processes and mechanisms underlying the interactions between pain, stress, and sex.
- Ultimately, a deeper understanding of these relationships is essential for developing personalized treatment options and improving the quality of life for individuals suffering from chronic visceral pain and related disorders.
Review date not set.
How we reviewed this article:
Latest on: