5 Triggers for Abdominal Pain in Obstructive Bowel Disorders (OBD)
Discover the 5 key triggers of abdominal pain in obstructive bowel disorders and learn how to manage them for improved gut health and comfort.
In This Article:
Key Points
- Obstructive bowel disorders (OBD) are characterized by abdominal pain due to lumen distention caused by mechanical or functional obstructions in the gut.
- Acute and chronic pain in bowel obstruction (BO) can be caused by clustered contractions, increased intraluminal pressure, and ischemia in severe cases.
- Recent studies have shown that visceral sensitivity is heightened in BO, which may be a key mechanism behind chronic abdominal pain.
- Lumen distension in BO can alter gene expression in the distended bowel, leading to the development of visceral hypersensitivity through mechano-transcription of nociceptive and inflammatory mediators.
- Mechanical stretch-induced changes in gene expression and channel functions in primary sensory neurons, as well as the activation of nociceptors by inflammatory mediators, may be the main mechanisms behind visceral hypersensitivity and abdominal pain in OBD.
Obstructive Bowel Disorders: Causes, Symptoms, and Pain Mechanisms
Introduction: The Big Picture
Obstructive Bowel Disorders (OBD) are serious conditions that can lead to significant health problems, including hospitalization and even death A Trusted Source Wells, C. I., O’Grady, G., and Bissett, I. P. (2017). Acute colonic pseudo-obstruction: a systematic review of aetiology and mechanisms.World J. Gastroenterol.23, 5634–5644. doi: 10.3748/wjg.v23.i30.5634 PubMed AbstractCrossRef Full TextGoogle Scholar .
In the United States alone, more than 300,000 people are admitted to hospitals annually due to mechanical bowel obstruction (BO), a major type of OBD.
This results in nearly 30,000 deaths and medical costs exceeding $3 billion each year A Trusted Source Cappell, M. S., and Batke, M. (2008). Mechanical obstruction of the small bowel and colon.Med. Clin. North Am.92, 575–597, viii. doi: 10.1016/j.mcna.2008.01.003 PubMed AbstractCrossRef Full TextGoogle Scholar .
Understanding Mechanical Bowel Obstruction: The Main Culprit
Mechanical BO, which can be caused by various factors, including adhesions and cancers, is categorized into different types: partial or complete, and simple or closed loop.
While surgery is often required for complete and closed-loop obstructions, partial simple obstructions can typically be managed with less invasive methods.
Functional Obstruction: The Invisible Enemy
Unlike mechanical BO, functional obstruction is not caused by a physical blockage.
Instead, it results from neuromuscular dysfunction in the gastrointestinal (GI) tract, leading to symptoms similar to those of mechanical BO A Trusted Source De Giorgio, R., Cogliandro, R. F., Barbara, G., Corinaldesi, R., and Stanghellini, V. (2011). Chronic intestinal pseudo-obstruction: clinical features, diagnosis, and therapy.Gastroenterol. Clin. North Am.40, 787–807. doi: 10.1016/j.gtc.2011.09.005 PubMed AbstractCrossRef Full TextGoogle Scholar .
Symptoms and Pain: The Body's Alarm System
Abdominal pain, nausea, vomiting, and constipation are common symptoms of OBD, often caused by gut motility dysfunction A Trusted Source Gore, R. M., Silvers, R. I., Thakrar, K. H., Wenzke, D. R., Mehta, U. K., Newmark, G. M., et al. (2015). Bowel obstruction.Radiol. Clin. North Am.53, 1225–1240. doi: 10.1016/j.rcl.2015.06.008 PubMed AbstractCrossRef Full TextGoogle Scholar .

In cases of mechanical BO, abdominal pain is usually the main reason for hospital visits.
This pain can be colicky or persistent, depending on the type and duration of the obstruction A Trusted Source Ripamonti, C., and Mercadante, S. (2004). “Pathophysiology and management of malignant bowel obstruction,” inTextbook of Palliative Medicine, 3rd Edn, eds N. I. Cherny, M. Fallon, S. Kaasa, R. K. Portenoy, and D. Currow (New York, NY: Oxford University Press), 496–506.Google Scholar .
Mechanisms of Pain: Getting to the Root of the Problem
Recent studies have shown that visceral hypersensitivity is a key mechanism behind chronic abdominal pain in BO A Trusted Source Huang, T. Y., and Hanani, M. (2005). Morphological and electrophysiological changes in mouse dorsal root ganglia after partial colonic obstruction.Am. J. Physiol. Gastrointest. Liver Physiol.289, G670–G678. doi: 10.1152/ajpgi.00028.2005 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Lin, Y. M., Fu, Y., Winston, J., Radhakrishnan, R., Sarna, S. K., Huang, L. M., et al. (2017b). Pathogenesis of abdominal pain in bowel obstruction: role of mechanical stress-induced upregulation of nerve growth factor in gut smooth muscle cells.Pain158, 583–592. doi: 10.1097/j.pain.0000000000000797 PubMed AbstractCrossRef Full TextGoogle Scholar .
Visceral hypersensitivity, and increased sensitivity in the internal organs, can result in chronic pain.
Understanding the mechanisms behind this hypersensitivity and the associated pain is crucial for developing targeted therapies to relieve the suffering of those with OBD.
Abdominal Pain in Bowel Obstruction: A Neurobiological Approach
When bowel obstruction (BO) occurs, the abdominal pain experienced is mainly of visceral origin, which is distinct from somatic pain.
Visceral pain is usually dull, poorly defined, and often referred to the overlying skin of the abdominal wall, with referred pain resulting from the convergence of somatic and visceral afferents upon sensory neurons in the same spinal segments A Trusted Source Sengupta, J. N. (2009). Visceral pain: the neurophysiological mechanism.Handb. Exp. Pharmacol.194, 31–74. doi: 10.1007/978-3-540-79090-7_2PubMed AbstractCrossRef Full TextGoogle Scholar .
In cases of large bowel obstruction (LBO), pain may be referred to the mid or hypogastrium A Trusted Source Huang, T. Y., and Hanani, M. (2005). Morphological and electrophysiological changes in mouse dorsal root ganglia after partial colonic obstruction.Am. J. Physiol. Gastrointest. Liver Physiol.289, G670–G678. doi: 10.1152/ajpgi.00028.2005 PubMed AbstractCrossRef Full TextGoogle Scholar .
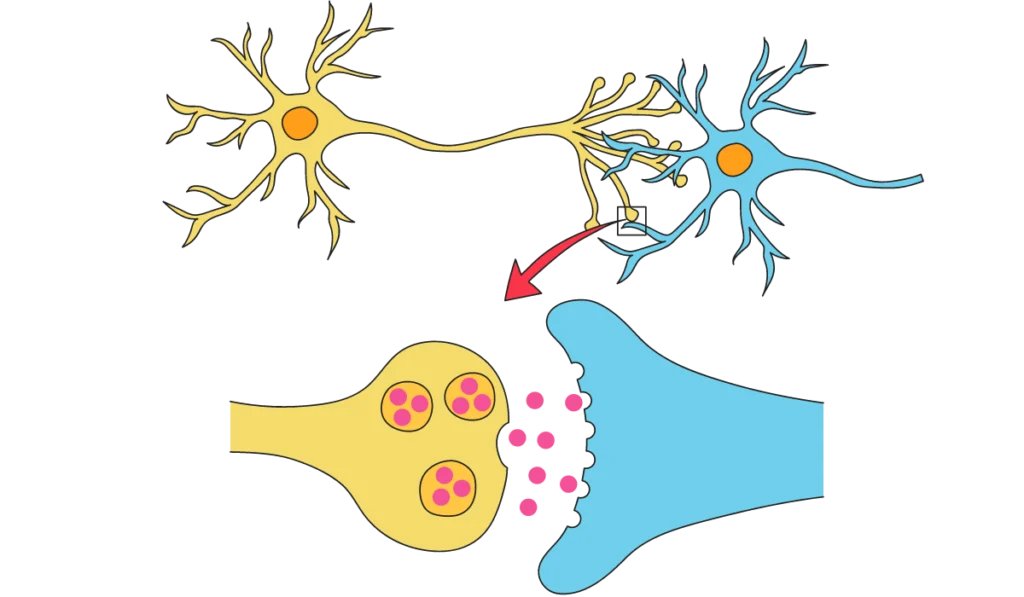
Nociceptors, the sensory receptors for pain, are found in various layers of the gut, and when activated, they send signals through primary afferent nerves to the dorsal root ganglia (DRG), which then synapse with second-order neurons in the spinal cord.
This initiates the central processing of sensory information and the experience of pain A Trusted Source Greenwood-Van Meerveld, B., Prusator, D. K., and Johnson, A. C. (2015). Animal models of gastrointestinal and liver diseases. Animal models of visceral pain: pathophysiology, translational relevance, and challenges.Am. J. Physiol. Gastrointest. Liver Physiol.308, G885–G903. doi: 10.1152/ajpgi.00463.2014 PubMed AbstractCrossRef Full TextGoogle Scholar .
Visceral sensitization of the peripheral and central pathways is now recognized as a key mechanism in the development of abdominal pain A Trusted Source Azpiroz, F., Bouin, M., Camilleri, M., Mayer, E. A., Poitras, P., Serra, J., et al. (2007). Mechanisms of hypersensitivity in IBS and functional disorders.Neurogastroenterol. Motil.19, 62–88. doi: 10.1111/j.1365-2982.2006.00875.x PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Zhou, Y. Y., Wanner, N. J., Xiao, Y., Shi, X. Z., Jiang, X. H., Gu, J. G., et al. (2012). Electroacupuncture alleviates stress-induced visceral hypersensitivity through an opioid system in rats.World J. Gastroenterol.18, 7201–7211. doi: 10.3748/wjg.v18.i48.7201 PubMed AbstractCrossRef Full TextGoogle Scholar .
Various peripheral mediators, such as neurotrophins (NT) including nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF), prostaglandins like PGE2, and 5-hydroxytryptamine (5-HT), can sensitize the processes of sensation and transduction in afferent neurons by lowering nociceptor firing thresholds.
This sensitization is crucial to the development of visceral pain in gastrointestinal (GI) disorders A Trusted Source Pezet, S., and McMahon, S. B. (2006). Neurotrophins: mediators and modulators of pain.Annu. Rev. Neurosci.29, 507–538. doi: 10.1146/annurev.neuro.29.051605.112929 CrossRef Full TextGoogle Scholar .
Abdominal Pain in Bowel Obstruction: A Closer Look
Acute abdominal pain in bowel obstruction (BO) is a common yet intricate phenomenon, typically accompanied by abdominal distension.
This pain is often more intense in the lower gastrointestinal tract, particularly in the colon.
Colicky pain is a characteristic feature of acute BO A Trusted Source Gore, R. M., Silvers, R. I., Thakrar, K. H., Wenzke, D. R., Mehta, U. K., Newmark, G. M., et al. (2015). Bowel obstruction.Radiol. Clin. North Am.53, 1225–1240. doi: 10.1016/j.rcl.2015.06.008PubMed AbstractCrossRef Full TextGoogle Scholar .
Mechanisms of Acute Abdominal Pain in BO
The nociceptive mechanisms underlying acute pain in BO are not entirely clear.
It is thought that the pain might arise from the activation of mechanosensitive nociceptors in the visceral afferents due to increased intraluminal pressure resulting from clustered contractions.
In extreme cases, such as closed-loop obstruction, ischemia and inflammatory mediators can further activate the visceral afferents via chemical receptors, thereby contributing to the pain experienced.
Gut Motility and Colicky Pain: The Interplay in BO
Gut motility is significantly altered in both small bowel obstruction (SBO) and large bowel obstruction (LBO).
In SBO, motility is inhibited in the segment distal to the occlusion while temporarily increased in the segment proximal to the occlusion.
This is likely a result of enhanced peristalsis stimulated by the intraluminal mechanical retention at the site of obstruction, leading to ascending excitation of contractile activities in the proximal segment and descending inhibition in the distal segment A Trusted Source Prihoda, M., Flatt, A., and Summers, R. W. (1984). Mechanisms of motility changes during acute intestinal obstruction in the dog.Am. J. Physiol.247, G37–G42. doi: 10.1152/ajpgi.1984.247.1.G37 PubMed AbstractCrossRef Full TextGoogle Scholar .
This can result in clustered contraction patterns in the distended proximal segment, with contractions of high amplitude and rapid propagation at nearly 1 cm/s.
Motor activity is also heightened in the early hours of LBO, especially if the obstruction is in the distal colon.
These activities substantially increase the intraluminal pressure, potentially stimulating mechanoreceptors in the sensory neurons, and hence, leading to pain A Trusted Source Silen, W. (2005). “Acute intestinal obstruction,” inHarrison’s Principles of Internal Medicine, 16th Edn, eds D. L. Longo, A. S. Fauci, D. L. Kasper, S. L. Hauser, J. Jameson, and J. Loscalzo (New York, NY: McGraw-Hill), 1803–1805.Google Scholar .
Exploring the Mechanisms of Colicky Pain
An in-depth investigation into the mechanotransduction signaling in the visceral afferents may reveal the intricacies of colicky pain in BO.
Several mechanoreceptors have been identified in the gastrointestinal tract, such as the degenerin/epithelial sodium channel (DEG/ENaC) family, the transient receptor potential (TRP) family of ion channels, including TRPV4, and the newly identified Piezo channels A Trusted Source Volkers, L., Mechioukhi, Y., and Coste, B. (2015). Piezo channels: from structure to function.Pflugers Arch.467, 95–99. doi: 10.1007/s00424-014-1578-z PubMed AbstractCrossRef Full TextGoogle Scholar .
Understanding these mechanisms may provide insights into the root cause of colicky pain in BO.
Ischemia's Role in Abdominal Pain During BO
Intraluminal pressure increases in BO can lead to local ischemia in the obstructed bowel, potentially playing a role in acute abdominal pain.
While high intraluminal pressures might not be sufficient to cause transmural ischemia, other factors such as external compression of the bowel or its mesentery can compromise blood supply, leading to abdominal pain.
Strangulation-associated ischemia can occur in closed-loop obstructions, potentially resulting in severe complications such as perforation and peritonitis.
These complications may activate afferent neurons through acid-sensitive ion channels (ASIC), TRPV1, and P2X3 in the sensory nerve endings A Trusted Source Feuerstadt, P., and Brandt, L. J. (2015). Update on colon ischemia: recent insights and advances.Curr. Gastroenterol. Rep.17:45. doi: 10.1007/s11894-015-0469-6 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Oglat, A., and Quigley, E. M. (2017). Colonic ischemia: usual and unusual presentations and their management.Curr. Opin. Gastroenterol.33, 34–40. doi: 10.1097/MOG.0000000000000325 PubMed AbstractCrossRef Full TextGoogle Scholar .
The Evolution of Pain in Prolonged BO
As obstruction persists beyond 12 to 24 hours, gut motor activity begins to decrease, transforming acute colicky pain into more chronic persistent pain.
This is a major concern in patients with chronic partial obstructions, such as inoperable or malignant obstructions (MBO).
Research indicates that visceral sensitivity intensifies within 72 hours of obstruction, contributing to chronic abdominal pain in OBD A Trusted Source Lin, Y. M., Fu, Y., Winston, J., Radhakrishnan, R., Sarna, S. K., Huang, L. M., et al. (2017b). Pathogenesis of abdominal pain in bowel obstruction: role of mechanical stress-induced upregulation of nerve growth factor in gut smooth muscle cells.Pain158, 583–592. doi: 10.1097/j.pain.0000000000000797 PubMed AbstractCrossRef Full TextGoogle Scholar .
Pain in Bowel Obstruction: The Role of Mechanical Stretch
When our bowels get obstructed, it can lead to a condition known as bowel obstruction distress (OBD), marked by gut stretching and distending.
This stretch is a significant player in the abdominal pain we experience during chronic obstructions like malignant bowel obstruction (MBO) A Trusted Source Postier, R. G., and Squires, R. A. (2007). “Acute abdomen. Chapter 45,” inSebiston Textbook of Surgery, 18th Edn, ed. C. M. Townsend (Philadelphia, PA: Saunders Elsevier). .
The Impact of Mechanical Stretch on Gene Expression
Recent studies have dived deep into how this stretching affects our genes, especially the ones responsible for pain.
The hypothesis was that when our gut stretches, it might trigger specific genes to produce pain mediators, thereby heightening sensitivity and causing pain in OBD A Trusted Source Shi, X. Z. (2017). Mechanical regulation of gene expression in gut smooth muscle cells.Front. Physiol.8:1000. doi: 10.3389/fphys.2017.01000 CrossRef Full TextGoogle Scholar.
This was put to the test using a rat model where a partial colon obstruction was created.
The results identified several gene groups altered by this stretch, including those related to inflammation, growth, and pain mediators like COX-2, NGF, and BDNF A Trusted Source Shi, X. Z., Lin, Y. M., Powell, D. W., and Sarna, S. K. (2011). Pathophysiology of motility dysfunction in bowel obstruction: role of stretch-induced COX-2.Am. J. Physiol. Gastrointest. Liver Physiol.300, G99–G108. doi: 10.1152/ajpgi.00379.2010 PubMed AbstractCrossRef Full TextGoogle Scholar .
Focusing on COX-2: A Key Pain Mediator
A closer look at COX-2 revealed that mechanical stretch particularly influences its gene expression in our gut's smooth muscle cells (SMCs).
Immunohistochemical studies highlighted that this increase was specific to the SMCs and not other layers of our gut.
Further investigation revealed that specific proteins and kinases, including MAPK ERK, p38, JNK, and PKC (especially PKCdelta), are crucial in this mechano-transcription of COX-2 in gut SMCs A Trusted Source Li, F., Lin, Y. M., Sarna, S. K., and Shi, X. Z. (2012a). Cellular mechanism of mechanotranscription in colonic smooth muscle cells.Am. J. Physiol. Gastrointest. Liver Physiol.303, G646–G656. doi: 10.1152/ajpgi.00440.2011 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Li, F., Sarna, S. K., and Shi, X. Z. (2012b). Roles of PKCs and PKD in mechanotranscription in colonic smooth muscle cells: inhibition of mechanotranscription as a potential treatment for motility dysfunction in obstructive disorders.Gastroenterology142:S-29. doi: 10.1016/S0016-5085(12)60115-2 CrossRef Full TextGoogle Scholar .
The Domino Effect: Stretch, COX-2, and Visceral Hypersensitivity
But how does all this lead to the intense abdominal pain in OBD?
Lin et al. A Trusted Source Lin, Y. M., Fu, Y., Wu, C. C., Xu, G. Y., Huang, L. Y., and Shi, X. Z. (2015). Colon distention induces persistent visceral hypersensitivity by mechanotranscription of pain mediators in colonic smooth muscle cells.Am. J. Physiol. Gastrointest. Liver Physiol.308, G434–G441. doi: 10.1152/ajpgi.00328.2014 PubMed AbstractCrossRef Full TextGoogle Scholar showed that stretching the colon increases COX-2 expression and subsequently, PGE2 production in colonic smooth muscle.
This increase in PGE2, a known pain mediator, results in heightened visceral sensitivity.
This sensitivity can last up to 3 days and is marked by an increase in the excitability of sensory neurons in the dorsal root ganglia (DRG).
However, it was found that by administering a COX-2 inhibitor, this chain of events could be interrupted, significantly reducing visceral hypersensitivity.
Decoding the Pain: How Neurotrophins Heighten Sensitivity in Bowel Obstruction
Pain in bowel obstructions (BO) isn’t just uncomfortable; it’s linked to a complex chain of reactions inside our bodies.
The culprits?
Neurotrophins like NGF and BDNF, are well-established pain mediators A Trusted Source Bielefeldt, K. (2006). “Neurochemical and molecular basis of peripheral sensitization,” inChronic Abdominal and Visceral Pain, eds P. J. Pasricha, W. D. Willis, and G. F. Gebhart (Boca Raton, FL: Informa Healthcare), 67–83. doi: 10.3109/9781420004434-7 CrossRef Full TextGoogle Scholar .
Zooming In: NGF’s Role in the Game
In BO, a significant uptick of NGF mRNA and protein was found in the stretched colonic smooth muscle cells (SMC) of rats, while the opposite side remained unaffected A Trusted Source Lin, Y. M., Fu, Y., Winston, J., Radhakrishnan, R., Sarna, S. K., Huang, L. M., et al. (2017b). Pathogenesis of abdominal pain in bowel obstruction: role of mechanical stress-induced upregulation of nerve growth factor in gut smooth muscle cells.Pain158, 583–592. doi: 10.1097/j.pain.0000000000000797 PubMed AbstractCrossRef Full TextGoogle Scholar .
This stretch and elevation of NGF led to hyperactive colon-projecting dorsal root ganglia (DRG) neurons, further amplifying visceral sensitivity.
What’s fascinating is when these neurons were exposed to media from the stretched muscle strips, their excitability shot up, but this effect was notably dampened by anti-NGF antibody.
This indicates the potent role of NGF in heightening neuron sensitivity.
BDNF's Entry: Adding Fuel to the Fire
Not to be outdone, BDNF too showed a dramatic rise in its mRNA and protein levels in the strained colonic SMC, causing a whirlwind of changes in the neurons of BO rats.
This included a marked drop in total K+ current and the transient inactivating A-type (IA) current in the colon neurons, all potentially leading to heightened sensitivity and pain A Trusted Source Fu, Y., Lin, Y. M., Winston, J. H., Radhakrishnan, R., Huang, L. M., and Shi, X. Z. (2018). Role of brain-derived neurotrophic factor in the pathogenesis of distention-associated abdominal pain in bowel obstruction.Neurogastroenterol. Motil.30:e13373. doi: 10.1111/nmo.13373 PubMed AbstractCrossRef Full TextGoogle Scholar .
Blocking BDNF’s receptor Trk B resulted in improved hyperalgesia, further underscoring BDNF’s role in this complex pain web A Trusted Source Lin, Y. M., Fu, Y., Radhakrishnan, R., Huang, L. Y., and Shi, X. Z. (2017a). Stretch-induced BDNF in colon smooth muscle plays a critical role in obstruction associated visceral hypersensitivity by altering Kv function in primary sensory neurons.Gastroenterology152(Suppl. 1), S203–S204. doi: 10.1016/S0016-5085(17)30986-1 CrossRef Full TextGoogle Scholar .

Unraveling the Unknown in Bowel Obstruction Pain
When it comes to bowel obstruction (BO), there's more than meets the eye.
Past research has revealed intriguing changes in satellite glia cells and dorsal root ganglia (DRG) neurons in chronic intestinal obstruction A Trusted Source Williams, T. H., Zhang, M. Q., and Jew, J. Y. (1993). Hypertrophy of rat sensory ganglion neurons following intestinal obstruction.Gastroenterology105, 8–14. doi: 10.1016/0016-5085(93)90004-VPubMed AbstractCrossRef Full TextGoogle Scholar .
Yet, the full picture of how these changes contribute to abdominal pain is still unclear.
In the fascinating world of partial colon obstruction, the research didn't show significant DRG neuron size changes within 7 days A Trusted Source Lin, Y. M., Fu, Y., Winston, J., Radhakrishnan, R., Sarna, S. K., Huang, L. M., et al. (2017b). Pathogenesis of abdominal pain in bowel obstruction: role of mechanical stress-induced upregulation of nerve growth factor in gut smooth muscle cells.Pain158, 583–592. doi: 10.1097/j.pain.0000000000000797 PubMed AbstractCrossRef Full TextGoogle Scholar .
However, it's proposed that the increase in glial coupling and DRG neuron size could play a crucial role in BO-related abdominal pain A Trusted Source Slugg, R. M., Meyer, R. A., and Campbell, J. N. (2000). Response of cutaneous A- and C-fiber nociceptors in the monkey to controlled-force stimuli.J. Neurophysiol.83, 2179–2191. doi: 10.1152/jn.2000.83.4.2179 PubMed AbstractCrossRef Full TextGoogle Scholar .
But wait, there's more.
The potential impact of mechanical stretch on enteric neurons and interstitial cells of Cajal is another aspect that deserves our attention A Trusted Source Wu, C. C., Lin, Y. M., Gao, J., Winston, J. H., Cheng, L. K., and Shi, X. Z. (2013). Are interstitial cells of Cajal involved in mechanical stress-induced gene expression and impairment of smooth muscle contractility in bowel obstruction?PLoS One8:e76222. doi: 10.1371/journal.pone.007622 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Lin, Y. M., Li, F., Choudhury, B., Winston, J. H., Sarna, S. K., and Shi, X. Z. (2014). Effects of mechanical stress on myenteric neurons in the colon.Gastroenterology146:S-91. doi: 10.1016/S0016-5085(14)60330-9 PubMed AbstractCrossRef Full TextGoogle Scholar.
Could this stretch be a culprit in sensory-motor dysfunction in OBD?
And what about its effect on extrinsic afferent nerve endings?
Time and further research will tell.
As we delve deeper into the mechanisms of mechano-transcription of pain mediators in the gut, we inch closer to uncovering potential therapeutic targets that could revolutionize the management of abdominal pain in OBD A Trusted Source Li, F., Lin, Y. M., Sarna, S. K., and Shi, X. Z. (2012a). Cellular mechanism of mechanotranscription in colonic smooth muscle cells.Am. J. Physiol. Gastrointest. Liver Physiol.303, G646–G656. doi: 10.1152/ajpgi.00440.2011 PubMed AbstractCrossRef Full TextGoogle Scholar .
The journey continues!
Discussion
- Obstructive Bowel Disorders (OBD) significantly affect the healthcare system, resulting in substantial hospital admissions and medical costs.
- Mechanical Bowel Obstruction (BO) is a primary type of OBD, which requires a comprehensive understanding of its causes, symptoms, and mechanisms to improve patient outcomes.
- The mechanisms behind the abdominal pain experienced in BO are complex and multifaceted, involving various pathways and mediators, including visceral hypersensitivity, mechanosensitive nociceptors, and neurotrophins such as NGF and BDNF.
- Recent research has highlighted the role of mechanical stretch in OBD, which affects gene expression related to inflammation, growth, and pain mediators, subsequently influencing pain mechanisms in OBD.
- The interplay between gut motility and colicky pain in BO is another area that requires further exploration to fully understand the intricacies of abdominal pain in OBD.
Conclusion
- OBD is a complex and serious condition that requires an in-depth understanding of its causes, symptoms, and mechanisms to improve patient outcomes and reduce the burden on the healthcare system.
- Mechanical BO, as a significant type of OBD, encompasses a range of factors that contribute to its onset and progression, including various causes, symptoms, and pain mechanisms.
- Abdominal pain in BO is a critical aspect that necessitates thorough investigation to identify the root causes and develop targeted therapies to alleviate patient suffering.
- The insights gained from recent research on the role of mechanical stretch and its impact on gene expression, as well as the intricate mechanisms underlying colicky pain and gut motility, are pivotal in unraveling the complexities of OBD.
- Ultimately, ongoing research and a comprehensive approach are essential to unravel the complexities of OBD, paving the way for innovative and effective treatment strategies that can significantly improve the quality of life for patients suffering from this condition.
Review date not set.
How we reviewed this article:
Latest on:





