Heart Health Myths Linked to Gut Microbiota Debunked
Discover the truth behind heart health with our expert myth-busting guide on gut microbiota’s real impact. Stay informed, stay healthy!

Gut bacteria, more than just digestive aides, play a key role in heart health.
They influence metabolism, inflammation, and immune responses—vital factors in heart disease.
Understanding this intricate gut-heart link is crucial, as their byproducts can impact heart disease's course.
In This Article:
Key Points
- Gut bacteria, including bacteria, fungi, viruses, and protozoa, play a crucial role in heart health by influencing metabolism, inflammation, and immune responses.
- The balance of gut bacteria, indicated by the Firmicutes/Bacteroidetes ratio, is important for overall health.
- Gut bacteria can produce byproducts like trimethylamine N-oxide (TMAO), which can impact the course of heart disease and increase the risk of cardiovascular issues.
- The virome, including phages and viruses, is linked to cardiovascular disease and may act as potential risk markers.
- Fungi, such as Mucor spp., may have associations with healthier artery measurements and potentially lower cardiovascular risks.
- Gut metabolites, such as short-chain fatty acids (SCFAs) produced by gut bacteria from dietary fiber, can have positive effects on health, while TMAO may raise disease risk.
- Bile acids, traditionally known for their role in fat digestion, can influence the immune system, metabolism, and communication with gut microorganisms.
- Polyamines, such as spermidine, can support better heart function and foster beneficial bacteria in the gut.
Gut Guardians: Decoding Our Microbial Partners in Health and Disease
The bustling community of over 100 trillion microbes in our bodies, including bacteria, fungi, viruses, and protozoa, is more than a mere passenger.
It's a driving force in our health, wielding control over digestion, immunity, and even heart health A Trusted SourcecRinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GAD, Gasbarrini A, et al. What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases.Microorganisms(2019) 7(1):14. doi: 10.3390/microorganisms7010014ccc PubMed AbstractCrossRef Full TextGoogle Scholar efn_note] A Trusted Source Cho I, Blaser MJ. The human microbiome: at the interface of health and disease.Nat Rev Genet(2012) 13:260–70. doi: 10.1038/nrg3182cccPubMed AbstractCrossRef Full TextGoogle Scholar[/efn_note].
Dubbed the human microbiota, these tiny tenants are particularly concentrated in the gut, orchestrating a myriad of vital functions: they fine-tune metabolism, bolster the intestinal barrier, manage hunger signals, and arm us against invaders A Trusted Source Yoo JY, Groer M, Dutra SVO, Sarkar A, McSkimming DI. Gut microbiota and immune system interactions.Microorganisms(2020) 8(10):1587. doi: 10.3390/microorganisms8101587 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Talapko J, Vcev A, Mestrovic T, Pustijanac E, Jukic M, Skrlec I. Homeostasis and dysbiosis of the intestinal microbiota: comparing hallmarks of a healthy state with changes in inflammatory bowel disease.Microorganisms(2022) 10(12):2405. doi: 10.3390/microorganisms10122405 PubMed AbstractCrossRef Full TextGoogle Scholar.
Each person harbors a unique microbiotic fingerprint.
No single blend spells perfect health; rather, diversity and balance are key A Trusted Source Afzaal M, Saeed F, Shah YA, Hussain M, Rabail R, Socol CT, et al. Human gut microbiota in health and disease: Unveiling the relationship.Front Microbiol(2022) 13:999001. doi: 10.3389/fmicb.2022.999001 PubMed AbstractCrossRef Full TextGoogle Scholar.
These microorganisms, living in symbiosis with us, form a resilient superorganism with the major players, Firmicutes and Bacteroidetes, leading the pack in a healthy adult gut A Trusted Source Salvucci E. The human-microbiome superorganism and its modulation to restore health.Int J Food Sci Nutr(2019) 70:781–95. doi: 10.1080/09637486.2019.1580682 PubMed AbstractCrossRef Full TextGoogle Scholar.
Our lifestyle, diet, and even social interactions can nudge this microbial mix, hinting at their adaptive nature A Trusted Source Fassarella M, Blaak EE, Penders J, Nauta A, Smidt H, Zoetendal EG. Gut microbiome stability and resilience: elucidating the response to perturbations in order to modulate gut health.Gut(2021) 70:595–605. doi: 10.1136/gutjnl-2020-321747 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Wu HJ, Wu E. The role of gut microbiota in immune homeostasis and autoimmunity.Gut Microbes(2012) 3:4–14. doi: 10.4161/gmic.19320 PubMed AbstractCrossRef Full TextGoogle Scholar.
Disruption in this delicate balance—dysbiosis—triggers inflammation and immune misfires, contributing to a plethora of conditions, from gut disorders to heart disease and beyond A Trusted Source Martinez JE, Kahana DD, Ghuman S, Wilson HP, Wilson J, Kim SCJ, et al. Unhealthy lifestyle and gut dysbiosis: A better understanding of the effects of poor diet and nicotine on the intestinal microbiome.Front Endocrinol (Lausanne)(2021) 12:667066. doi: 10.3389/fendo.2021.667066 PubMed AbstractCrossRef Full TextGoogle Scholar.
The Firmicutes/Bacteroidetes ratio is gaining traction as a health indicator, a microbial meter of our well-being A Trusted Source Yang T, Santisteban MM, Rodriguez V, Li E, Ahmari N, Carvajal JM, et al. Gut dysbiosis is linked to hypertension.Hypertension(2015) 65:1331–40. doi: 10.1161/HYPERTENSIONAHA.115.05315 PubMed AbstractCrossRef Full TextGoogle Scholar.
Intriguingly, our gut residents have a say in cardiovascular health.
They churn out metabolites like TMAO from nutrients we consume, which scientists now link to heart disease risk A Trusted Source19. Rahman MM, Islam F, Or-Rashid MH, Mamun AA, Rahaman MS, Islam MM, et al. The gut microbiota (Microbiome) in cardiovascular disease and its therapeutic regulation.Front Cell Infect Microbiol(2022) 12:903570. doi: 10.3389/fcimb.2022.903570 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Almeida C, Barata P, Fernandes R. The influence of gut microbiota in cardiovascular diseases-a brief review.Porto BioMed J(2021) 6:e106. doi: 10.1097/j.pbj.0000000000000106PubMed AbstractCrossRef Full TextGoogle Scholar.
This understanding paves the way for groundbreaking treatments targeting these microbial processes A Trusted Source Honda K, Littman DR. The microbiota in adaptive immune homeostasis and disease.Nature(2016) 535:75–84. doi: 10.1038/nature18848 PubMed AbstractCrossRef Full TextGoogle Scholar.
Cardiovascular diseases claim millions of lives annually, influenced by genetics, environment, and, significantly, our gut microbiota A Trusted Source Liu Y, Dai M. Trimethylamine N-oxide generated by the gut microbiota is associated with vascular inflammation: new insights into atherosclerosis.Mediators Inflammation(2020) 2020:4634172. doi: 10.1155/2020/4634172 CrossRef Full TextGoogle Scholar A Trusted Source Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, Jensen BA, et al. Human gut microbes impact host serum metabolome and insulin sensitivity.Nature(2016) 535:376–81. doi: 10.1038/nature18646 PubMed AbstractCrossRef Full TextGoogle Scholar.
Obesity, diabetes, and metabolic syndrome—cardiovascular foes—are tied to an imbalanced gut ecosystem A Trusted Source Canfora EE, Meex RCR, Venema K, Blaak EE. Gut microbial metabolites in obesity, NAFLD and T2DM.Nat Rev Endocrinol(2019) 15:261–73. doi: 10.1038/s41574-019-0156-z PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Rahman MM, Islam F, Or-Rashid MH, Mamun AA, Rahaman MS, Islam MM, et al. The gut microbiota (Microbiome) in cardiovascular disease and its therapeutic regulation.Front Cell Infect Microbiol(2022) 12:903570. doi: 10.3389/fcimb.2022.903570 PubMed AbstractCrossRef Full TextGoogle Scholar.
TMAO, a gut-derived molecule, has emerged as a heart disease herald, with research spotlighting its precursors and the influence of diet on its levels A Trusted Source Almeida C, Barata P, Fernandes R. The influence of gut microbiota in cardiovascular diseases-a brief review.Porto BioMed J(2021) 6:e106. doi: 10.1097/j.pbj.0000000000000106 PubMed AbstractCrossRef Full TextGoogle Scholar.
Our exploration dives into the gut's role in heart health, eyeing the latest insights on TMAO as a heart risk biomarker, and the beneficial contributions of fatty acids and other gut-derived substances A Trusted Source Cho CE, Caudill MA. Trimethylamine-N-oxide: friend, foe, or simply caught in the cross-fire?Trends Endocrinol Metab(2017) 28:121–30. doi: 10.1016/j.tem.2016.10.005 PubMed AbstractCrossRef Full TextGoogle Scholar .
This trove of knowledge isn't just academic; it's a beacon for future heart-saving therapies.
Understanding and harnessing our internal microbial cosmos could lead to revolutionary ways to prevent and treat heart disease, a testament to the power residing within our own biology.

Gut Microbiota Ecology and Its Implication on Cardiovascular Diseases
Gut Bacteria: A New Frontier in Heart Health
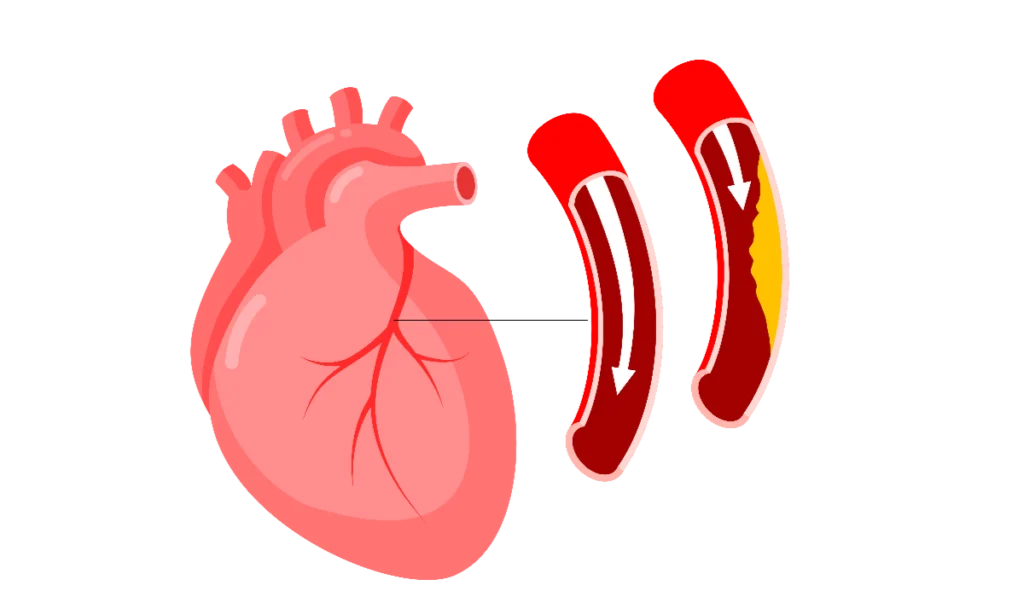
Beneath the surface of our everyday lives, trillions of bacteria dwell in our gut, silently orchestrating a multitude of processes that are crucial to our health.
They form a complex ecosystem with a profound influence on cardiovascular diseases (CVDs) such as heart attacks and strokes.
Research indicates that the specific makeup and diversity of our gut bacteria are tied to heart health, where imbalances may spell trouble A Trusted Source Witkowski M, Weeks TL, Hazen SL. Gut microbiota and cardiovascular disease.Circ Res(2020) 127:553–70. doi: 10.1161/CIRCRESAHA.120.316242 PubMed AbstractCrossRef Full TextGoogle Scholar efn_note] A Trusted Source Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers.Nature(2013) 500:541–6. doi: 10.1038/nature12506 PubMed AbstractCrossRef Full TextGoogle Scholar[/efn_note].
The gut barrier is our internal gatekeeper, a multilayered defense system keeping the potentially harmful contents of our gut from wandering where they shouldn't A Trusted Source Martel J, Chang SH, Ko YF, Hwang TL, Young JD, Ojcius DM. Gut barrier disruption and chronic disease.Trends Endocrinol Metab(2022) 33:247–65. doi: 10.1016/j.tem.2022.01.002 PubMed AbstractCrossRef Full TextGoogle Scholar.
When this barrier is compromised—a condition sometimes referred to as "leaky gut"—toxins can slip into the bloodstream, potentially triggering inflammation, a known accomplice in heart disease A Trusted Source Christovich A, Luo XM. Gut microbiota, leaky gut, and autoimmune diseases.Front Immunol(2022) 13:946248. doi: 10.3389/fimmu.2022.946248 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Inczefi O, Bacsur P, Resal T, Keresztes C, Molnar T. The influence of nutrition on intestinal permeability and the microbiome in health and disease.Front Nutr(2022) 9:718710. doi: 10.3389/fnut.2022.718710 PubMed AbstractCrossRef Full TextGoogle Scholar.
This inflammation is partly incited by substances like lipopolysaccharides (LPS), remnants of certain bacteria that, when free in the bloodstream, provoke a robust immune response.
They're suspected culprits in the leaky gut-CVD connection, although research is ongoing to unravel the complexities of this relationship A Trusted Source Mohammad S, Thiemermann C. Role of metabolic endotoxemia in systemic inflammation and potential interventions.Front Immunol(2020) 11:594150. doi: 10.3389/fimmu.2020.594150 PubMed AbstractCrossRef Full TextGoogle Scholar.
Intriguingly, our gut bacteria might affect heart health by influencing inflammation and metabolism A Trusted Source Xu H, Wang X, Feng W, Liu Q, Zhou S, Liu Q, et al. The gut microbiota and its interactions with cardiovascular disease.Microb Biotechnol(2020) 13:637–56. doi: 10.1111/1751-7915.13524 PubMed AbstractCrossRef Full TextGoogle Scholar.
Some bacteria produce inflammatory substances, contributing to conditions like atherosclerosis, while others may disrupt the balance of blood lipids or glucose control—known risk factors for CVD A Trusted Source Novakovic M, Rout A, Kingsley T, Kirchoff R, Singh A, Verma V, et al. Role of gut microbiota in cardiovascular diseases.World J Cardiol(2020) 12:110–22. doi: 10.4330/wjc.v12.i4.110 PubMed AbstractCrossRef Full TextGoogle Scholar.
Even arterial stiffness, a harbinger of cardiovascular trouble, might be traced back to the activities of gut microbes, particularly their production of short-chain fatty acids (SCFAs) in animal studies A Trusted Source Agnoletti D, Piani F, Cicero AFG, Borghi C. The gut microbiota and vascular aging: A state-of-the-art and systematic review of the literature.J Clin Med(2022) 11(12):3557. doi: 10.3390/jcm11123557 PubMed AbstractCrossRef Full TextGoogle Scholar.
It's a dynamic realm where gut bacteria could be both heroes and villains in the story of heart disease.
As scientists work to demystify the gut-heart connection, this knowledge holds the promise of novel preventive and therapeutic strategies against CVDs.

The Invisible Influence: How Viruses Within Us Could Shape Heart Health
Within every human resides an invisible population of viruses, collectively known as the viral microbiota, which includes a variety of viruses like bacteriophages and retroviruses A Trusted Source Cao Z, Sugimura N, Burgermeister E, Ebert MP, Zuo T, Lan P. The gut virome: A new microbiome component in health and disease.EBioMedicine(2022) 81:104113. doi: 10.1016/j.ebiom.2022.104113 PubMed AbstractCrossRef Full TextGoogle Scholar.
These viral inhabitants are not merely passengers; they can actively shape the landscape of our bodily microbiota A Trusted Source Mukhopadhya I, Segal JP, Carding SR, Hart AL, Hold GL. The gut virome: the 'missing link' between gut bacteria and host immunity?Therap Adv Gastroenterol(2019) 12:1756284819836620. doi: 10.1177/1756284819836620 PubMed AbstractCrossRef Full TextGoogle Scholar.
Bacteriophages, or phages for short, come in two main types: lytic, which kill their host cells, and lysogenic, which coexist more peacefully by integrating their DNA into the host's genome A Trusted Source Shamash M, Maurice CF. Phages in the infant gut: a framework for virome development during early life.ISME J(2022) 16:323–30. doi: 10.1038/s41396-021-01090-x PubMed AbstractCrossRef Full TextGoogle Scholar.
While some phages are harmful, others maintain harmony in our microbiome and defend against bacterial pathogens A Trusted Source Liang G, Bushman FD. The human virome: assembly, composition and host interactions.Nat Rev Microbiol(2021) 19:514–27. doi: 10.1038/s41579-021-00536-5 PubMed AbstractCrossRef Full TextGoogle Scholar.
Emerging research links these viral residents to cardiovascular diseases (CVD).
For instance, people with CVD show different viral patterns compared to those without, hinting that specific phages could be risk markers for heart issues A Trusted Source de Jonge PA, Wortelboer K, Scheithauer TPM, van den Born BH, Zwinderman AH, Nobrega FL, et al. Gut virome profiling identifies a widespread bacteriophage family associated with metabolic syndrome.Nat Commun(2022) 13:3594. doi: 10.1038/s41467-022-31390-5 PubMed AbstractCrossRef Full TextGoogle Scholar.
Studies like those by De Jonge PA et al. reveal that individuals with metabolic syndrome, a condition paving the way to heart disease, harbor a less diverse viral community, with particular viruses linked to key gut bacteria potentially impacting metabolic processes A Trusted Source de Jonge PA, Wortelboer K, Scheithauer TPM, van den Born BH, Zwinderman AH, Nobrega FL, et al. Gut virome profiling identifies a widespread bacteriophage family associated with metabolic syndrome.Nat Commun(2022) 13:3594. doi: 10.1038/s41467-022-31390-5 PubMed AbstractCrossRef Full TextGoogle Scholar .
Differences extend to patients with coronary heart disease (CHD), where the balance of viral families differs significantly from healthy individuals.
The presence of certain viruses, like those from the Microviridae family, may be influenced by diet or medical treatments, offering a unique snapshot of the viral ecosystem in heart disease A Trusted Source Schroder SL, Richter M, Schroder J, Frantz S, Fink A. Socioeconomic inequalities in access to treatment for coronary heart disease: A systematic review.Int J Cardiol(2016) 219:70–8. doi: 10.1016/j.ijcard.2016.05.066 PubMed AbstractCrossRef Full TextGoogle Scholar .
However, it’s clear that more exploration is needed to determine the exact nature of the connection between our inner viral world and heart health A Trusted Source Guo L, Hua X, Zhang W, Yang S, Shen Q, Hu H, et al. Viral metagenomics analysis of feces from coronary heart disease patients reveals the genetic diversity of the Microviridae.Virol Sin(2017) 32:130–8. doi: 10.1007/s12250-016-3896-0 PubMed AbstractCrossRef Full TextGoogle Scholar.
This exploration into the virome opens new doors for understanding how our internal viral universe impacts our well-being, particularly heart health, and could lead to novel diagnostics or treatments.
Mycobiome Mysteries: Can Fungi Influence Heart Disease Risk?
Our bodies are home to a microscopic ecosystem, including a variety of fungi ranging from yeasts to molds A Trusted Source Perez JC. Fungi of the human gut microbiota: Roles and significance.Int J Med Microbiol(2021) 311:151490. doi: 10.1016/j.ijmm.2021.151490 PubMed AbstractCrossRef Full TextGoogle Scholar.
While often overshadowed by bacteria, these fungi play vital roles in digestion and immune regulation A Trusted Source Dalamaga M, Zheng L, Liu J. Gut mycobiome as a promising preventive and therapeutic target for metabolic disorders.Metabol Open(2022) 13:100168. doi: 10.1016/j.metop.2022.100168 PubMed AbstractCrossRef Full TextGoogle Scholar.
But did you know they might also influence heart health?
Recent studies highlight a connection between fungi and cardiovascular diseases (CVD)—ailments of the heart and vessels.
Take Candida, a common yeast; it's found more frequently in those with heart issues, potentially due to the toxins it produces that can harm blood vessels A Trusted Source Giuliano S, Guastalegname M, Russo A, Falcone M, Ravasio V, Rizzi M, et al. Candida endocarditis: systematic literature review from 1997 to 2014 and analysis of 29 cases from the Italian Study of Endocarditis.Expert Rev Anti Infect Ther(2017) 15:807–18. doi: 10.1080/14787210.2017.1372749 PubMed AbstractCrossRef Full TextGoogle Scholar.
Molds like Aspergillus, too, are under scrutiny for their links to heart risks A Trusted Source Kalokhe AS, Rouphael N, El Chami MF, Workowski KA, Ganesh G, Jacob JT. Aspergillus endocarditis: a review of the literature.Int J Infect Dis(2010) 14:e1040–1047. doi: 10.1016/j.ijid.2010.08.005 PubMed AbstractCrossRef Full TextGoogle Scholar.
CVD isn't a stroke of bad luck; it has known triggers like atherosclerosis and high blood pressure A Trusted Source Rahman MM, Islam F, Or-Rashid MH, Mamun AA, Rahaman MS, Islam MM, et al. The gut microbiota (Microbiome) in cardiovascular disease and its therapeutic regulation.Front Cell Infect Microbiol(2022) 12:903570. doi: 10.3389/fcimb.2022.903570PubMed AbstractCrossRef Full TextGoogle Scholar.
Zooming in on atherosclerosis, research has tagged certain fungi, such as Mucor spp., with a surprising twist: they're associated with healthier artery measurements and could even mark a lower cardiovascular risk A Trusted Source Chacon MR, Lozano-Bartolome J, Portero-Otin M, Rodriguez MM, Xifra G, Puig J, et al. The gut mycobiome composition is linked to carotid atherosclerosis.Benef Microbes(2018) 9:185–98. doi: 10.3920/BM2017.0029 PubMed AbstractCrossRef Full TextGoogle Scholar.
High blood pressure, a major CVD red flag, also shows a fascinating fungal connection.
Fungal diversity in our bodies changes with health states; it goes up when conditions like hypertension kick in.
Fungi like Malassezia ramp up inflammation, while others like Mortierella might act protectively, akin to probiotics A Trusted Source Zou Y, Ge A, Lydia B, Huang C, Wang Q, Yu Y. Gut mycobiome dysbiosis contributes to the development of hypertension and its response to immunoglobulin light chains.Front Immunol(2022) 13:1089295. doi: 10.3389/fimmu.2022.1089295 PubMed AbstractCrossRef Full TextGoogle Scholar.
However, the fungal chapter in the CVD story isn't fully written.
More research is essential to unravel these complex biological relationships.
Until science paints a clearer picture, sticking to a heart-friendly lifestyle—balanced diet and regular exercise—remains a wise defense against CVD and its silent fungal influences.
Microscopic Allies: How Gut Metabolites Shape Our Health
Our gut is a chemical factory, transforming what we eat into molecules that chat with our immune system, sometimes soothing, sometimes stirring up trouble A Trusted Source Herrema H, Nieuwdorp M, Groen AK. Microbiome and cardiovascular disease.Handb Exp Pharmacol(2022) 270:311–34. doi: 10.1007/164_2020_356 PubMed AbstractCrossRef Full TextGoogle Scholar.
Beneficial substances like SCFAs boost health, while others like TMAO may raise disease risk A Trusted Source63. Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, et al. Health benefits and side effects of short-chain fatty acids.Foods(2022) 11(18):2863. doi: 10.3390/foods11182863PubMed AbstractCrossRef Full TextGoogle Scholar.
Unraveling these interactions is key to unlocking new health strategies.
Gut Feeling: The Mighty Molecules Behind Your Health
Your gut does more than digest your last meal.
It's home to trillions of microbes that churn out short-chain fatty acids (SCFAs) from the fiber we eat A Trusted Source Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, et al. Health benefits and side effects of short-chain fatty acids.Foods(2022) 11(18):2863. doi: 10.3390/foods11182863 PubMed AbstractCrossRef Full TextGoogle Scholar.
These tiny molecules, with less than six carbons, wield mighty powers over our well-being.
Picture your gut as a bustling metropolis where fiber is a favored currency.
When you feast on fiber-rich foods, your gut microbes get to work, fermenting these indigestible bits into SCFAs like acetate, propionate, and butyrate.
These are not just waste products; they're chemical messengers keeping your gut lining robust, damping down inflammation, and even helping control how much you eat A Trusted Source Feng W, Ao H, Peng C. Gut microbiota, short-chain fatty acids, and herbal medicines.Front Pharmacol(2018) 9:1354. doi: 10.3389/fphar.2018.01354 PubMed AbstractCrossRef Full TextGoogle Scholar.
Acetate, the most common SCFA, keeps the peace in your gut, preventing rogue bacteria from causing chaos and helps maintain an optimal pH A Trusted Source Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, et al. Health benefits and side effects of short-chain fatty acids.Foods(2022) 11(18):2863. doi: 10.3390/foods11182863 PubMed AbstractCrossRef Full TextGoogle Scholar.
Propionate, the mediator, may ward off diabetes by keeping blood sugar in check and has a say in how hungry you feel A Trusted Source Zhang Y, Li X, Huang G, Wang H, Chen H, Su Y, et al. Propionate stimulates the secretion of satiety hormones and reduces acute appetite in a cecal fistula pig model.Anim Nutr(2022) 10:390–8. doi: 10.1016/j.aninu.2022.06.003 PubMed AbstractCrossRef Full TextGoogle Scholar.
Butyrate, the energy provider, fuels your gut cells, keeping them healthy and vigilant against diseases like colon cancer A Trusted Source Geng HW, Yin FY, Zhang ZF, Gong X, Yang Y. Butyrate suppresses glucose metabolism of colorectal cancer cells via GPR109a-AKT signaling pathway and enhances chemotherapy.Front Mol Biosci(2021) 8:634874. doi: 10.3389/fmolb.2021.634874 PubMed AbstractCrossRef Full TextGoogle Scholar.
Beyond the gut, SCFAs may safeguard your heart by tackling inflammation and tweaking fat metabolism — think of them as your cardiovascular custodians A Trusted Source Rahman MM, Islam F, Or-Rashid MH, Mamun AA, Rahaman MS, Islam MM, et al. The gut microbiota (Microbiome) in cardiovascular disease and its therapeutic regulation.Front Cell Infect Microbiol(2022) 12:903570. doi: 10.3389/fcimb.2022.903570 PubMed AbstractCrossRef Full TextGoogle Scholar.
They're also emerging as potential allies against neurodegenerative diseases like Alzheimer's A Trusted Source Wang C, Zheng D, Weng F, Jin Y, He L. Sodium butyrate ameliorates the cognitive impairment of Alzheimer's disease by regulating the metabolism of astrocytes.Psychopharmacol (Berl)(2022) 239:215–27. doi: 10.1007/s00213-021-06025-0 CrossRef Full TextGoogle Scholar.
Interestingly, the journey of SCFAs doesn't end in the gut.
They seep into your bloodstream and travel to the liver and beyond, pulling strings in lipid biosynthesis and glucose production — essential processes for your body's energy economy A Trusted Source Feng W, Ao H, Peng C. Gut microbiota, short-chain fatty acids, and herbal medicines.Front Pharmacol(2018) 9:1354. doi: 10.3389/fphar.2018.01354 PubMed AbstractCrossRef Full TextGoogle Scholar.
Along the way, they interact with specialized receptors to influence your genes and immune system A Trusted Source Tan J, McKenzie C, Potamitis M, Thorburn AN, Mackay CR, Macia L. The role of short-chain fatty acids in health and disease.Adv Immunol(2014) 121:91–119. doi: 10.1016/B978-0-12-800100-4.00003-9 PubMed AbstractCrossRef Full TextGoogle Scholar.
Decoding TMAO: A Gut Microbiota Metabolite with a Heart of Darkness
Your gut is teeming with bacteria that do more than just help digest your dinner.
These tiny microbes also produce a compound called trimethylamine N-oxide (TMAO) that might affect your heart's health more than you realize.
Here's the lowdown: when you tuck into a steak, an omelet, or a slice of salmon, your gut bacteria get busy breaking down choline, lecithin, and carnitine—nutrients abundant in these foods.
The result? TMAO.
It starts as TMA in your colon, then hits your liver, where it's transformed into TMAO and released into your body A Trusted Source Cho CE, Caudill MA. Trimethylamine-N-oxide: friend, foe, or simply caught in the cross-fire?Trends Endocrinol Metab(2017) 28:121–30. doi: 10.1016/j.tem.2016.10.005 PubMed AbstractCrossRef Full TextGoogle Scholar.
This molecule doesn't just float idly in your bloodstream; it gets down to business influencing your cells and organs.
When TMAO strolls into your arteries, it's not always the best guest.
It can settle into macrophages, the cells that gobble up cholesterol, triggering them to hoard cholesterol and become foam cells.
These cells are like little blobs of fat clogging up your arteries, a classic move in the atherosclerosis playbook—
where arteries get stiff and narrow, upping your risk for heart attacks and strokes A Trusted Source77. Yang S, Li X, Yang F, Zhao R, Pan X, Liang J, et al. Gut microbiota-dependent marker TMAO in promoting cardiovascular disease: inflammation mechanism, clinical prognostic, and potential as a therapeutic target.Front Pharmacol(2019) 10:1360. doi: 10.3389/fphar.2019.01360PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source78. Matsuzawa Y, Nakahashi H, Konishi M, Sato R, Kawashima C, Kikuchi S, et al. Microbiota-derived trimethylamine N-oxide predicts cardiovascular risk after STEMI.Sci Rep(2019) 9:11647. doi: 10.1038/s41598-019-48246-6PubMed AbstractCrossRef Full TextGoogle Scholar.
But TMAO doesn't stop there.
It's also involved in the cascade of signals that make your blood more likely to clot and impairs the process of shipping excess cholesterol out of your body A Trusted Source80. Bordoni L, Samulak JJ, Sawicka AK, Pelikant-Malecka I, Radulska A, Lewicki L, et al. Trimethylamine N-oxide and the reverse cholesterol transport in cardiovascular disease: a cross-sectional study.Sci Rep(2020) 10:18675. doi: 10.1038/s41598-020-75633-1 PubMed AbstractCrossRef Full TextGoogle Scholar.
High TMAO levels in the blood could spell trouble, with studies linking them to a greater risk of heart issues A Trusted Source Cho CE, Caudill MA. Trimethylamine-N-oxide: friend, foe, or simply caught in the cross-fire?Trends Endocrinol Metab(2017) 28:121–30. doi: 10.1016/j.tem.2016.10.005 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Matsumoto T, Kojima M, Takayanagi K, Taguchi K, Kobayashi T. Role of S-equol, indoxyl sulfate, and trimethylamine N-oxide on vascular function.Am J Hypertens(2020) 33:793–803. doi: 10.1093/ajh/hpaa053 PubMed AbstractCrossRef Full TextGoogle Scholar.
It's not all doom and gloom, though.
TMAO seems to wear multiple hats, potentially playing roles in regulating how your gut works, how your body uses energy, and even how your blood vessels function A Trusted Source Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease.Nature(2011) 472:57–63. doi: 10.1038/nature09922 PubMed AbstractCrossRef Full TextGoogle Scholar.
The plot thickens as scientists uncover that TMAO levels might be a crystal ball for heart health, hinting at the likelihood of heart attacks or strokes A Trusted Source Heianza Y, Ma W, Manson JE, Rexrode KM, Qi L. Gut microbiota metabolites and risk of major adverse cardiovascular disease events and death: A systematic review and meta-analysis of prospective studies.J Am Heart Assoc(2017) 6(7):e004947. doi: 10.1161/JAHA.116.004947 PubMed AbstractCrossRef Full TextGoogle Scholar.
By measuring TMAO in your blood or urine, doctors could potentially flag high-risk cases for cardiovascular diseases (CVD) A Trusted Source Ma J, Li H. The role of gut microbiota in atherosclerosis and hypertension.Front Pharmacol(2018) 9:1082. doi: 10.3389/fphar.2018.01082 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Thomas MS, Fernandez ML. Trimethylamine N-oxide (TMAO), diet and cardiovascular disease.Curr Atheroscler Rep(2021) 23:12. doi: 10.1007/s11883-021-00910-x PubMed AbstractCrossRef Full TextGoogle Scholar.
The Inside Scoop: How Bile Acids Impact Your Gut and Heart Health
Bile acids (BAs) aren't just about digesting your fries anymore.
These molecules, primarily known for breaking down fats in your gut, have leveled up their game A Trusted Source Di Ciaula A, Garruti G, Lunardi Baccetto R, Molina-Molina E, Bonfrate L, Wang DQ, et al. Bile acid physiology.Ann Hepatol(2017) 16 Suppl 1:S4–S14. doi: 10.5604/01.3001.0010.5493 CrossRef Full TextGoogle Scholar.
Scientists are buzzing about how BAs are now linked to the immune system, metabolism, and even how they communicate with the microorganisms in your gut A Trusted Source Alpuim Costa D, Nobre JG, Batista MV, Ribeiro C, Calle C, Cortes A, et al. Human microbiota and breast cancer-is there any relevant link?-A literature review and new horizons toward personalised medicine.Front Microbiol(2021) 12:584332. doi: 10.3389/fmicb.2021.584332 PubMed AbstractCrossRef Full TextGoogle Scholar.
Imagine BAs as your body's natural detergents, with their core ingredient being cholesterol.
They're created in your liver, stored in your gallbladder, and then released into your intestines when you eat.
There are two types: primary and secondary.
Primary BAs like cholic acid are made in the liver, while secondary BAs are the creation of your gut's bacteria and are a bit different in their functions A Trusted Source Alpuim Costa D, Nobre JG, Batista MV, Ribeiro C, Calle C, Cortes A, et al. Human microbiota and breast cancer-is there any relevant link?-A literature review and new horizons toward personalised medicine.Front Microbiol(2021) 12:584332. doi: 10.3389/fmicb.2021.584332 PubMed AbstractCrossRef Full TextGoogle Scholar.
But here's the cool part: BAs are not just digestive aids; they double as hormones.
They can chat with receptors like the farnesoid X receptor (FXR) and G Protein-coupled membrane receptor 5 (TGR5), telling your body to dial down fat oxidation and inflammation in blood vessels A Trusted Source Wang Z, Zhao Y. Gut microbiota derived metabolites in cardiovascular health and disease.Protein Cell(2018) 9:416–31. doi: 10.1007/s13238-018-0549-0PubMed AbstractCrossRef Full TextGoogle Scholar.
And it gets more interesting—BAs can boss around the bacteria in your gut.
Depending on their type, they can act as enforcers, promoting or inhibiting bacterial growth, even affecting those linked to disease A Trusted Source An C, Chon H, Ku W, Eom S, Seok M, Kim S, et al. Bile acids: major regulator of the gut microbiome.Microorganisms(2022) 10(9):1792. doi: 10.3390/microorganisms10091792 PubMed AbstractCrossRef Full TextGoogle Scholar efn_note] A Trusted Source Quinn RA, Melnik AV, Vrbanac A, Fu T, Patras KA, Christy MP, et al. Global chemical effects of the microbiome include new bile-acid conjugations.Nature(2020) 579:123–9. doi: 10.1038/s41586-020-2047-9 PubMed AbstractCrossRef Full TextGoogle Scholar[/efn_note].
BAs are like bouncers at the club of your gut, deciding which bacterial species get to thrive and which don't make the cut.
Moreover, BAs are like trainers for your gut lining, ensuring it's strong enough to keep harmful substances from sneaking into your bloodstream A Trusted Source Ghosh S, Whitley CS, Haribabu B, Jala VR. Regulation of intestinal barrier function by microbial metabolites.Cell Mol Gastroenterol Hepatol(2021) 11:1463–82. doi: 10.1016/j.jcmgh.2021.02.007 PubMed AbstractCrossRef Full TextGoogle Scholar.
Plus, there's chatter about secondary BAs being the good guys, with some evidence pointing to their anti-inflammatory and anti-cancer vibes A Trusted Source Yang R, Qian L. Research on gut microbiota-derived secondary bile acids in cancer progression.Integr Cancer Ther(2022) 21:15347354221114100. doi: 10.1177/15347354221114100 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Zhou C, Wang Y, Li C, Xie Z, Dai L. Amelioration of colitis by a gut bacterial consortium producing anti-inflammatory secondary bile acids.Microbiol Spectr(2023) 11:e0333022. doi: 10.1128/spectrum.03330-22 PubMed AbstractCrossRef Full TextGoogle Scholar.
Yet, it's not all about the good stuff.
When the balance tips, and there's an excess of secondary BAs, your heart might be at risk.
Researchers are eyeing this BA balance as a potential culprit in cardiovascular diseases (CVD) A Trusted Source Wang Z, Zhao Y. Gut microbiota derived metabolites in cardiovascular health and disease.Protein Cell(2018) 9:416–31. doi: 10.1007/s13238-018-0549-0PubMed AbstractCrossRef Full TextGoogle Scholar.
Unlocking Heart Health: The Power of Polyamines
Polyamines like cadaverine, putrescine, and spermidine may sound morbid, but they play a surprising role in our health.
Created by bacteria, these compounds can be a bit smelly, thanks to their presence in decomposing matter.
Cadaverine comes from the amino acid L-lysine A Trusted Source Yamamoto Y, Miwa Y, Miyoshi K, Furuyama J, Ohmori H. The Escherichia coli ldcC gene encodes another lysine decarboxylase, probably a constitutive enzyme.Genes Genet Syst(1997) 72:167–72. doi: 10.1266/ggs.72.167 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Park YK, Bearson B, Bang SH, Bang IS, Foster JW. Internal pH crisis, lysine decarboxylase and the acid tolerance response of Salmonella typhimurium.Mol Microbiol(1996) 20:605–11. doi: 10.1046/j.1365-2958.1996.5441070.x PubMed AbstractCrossRef Full TextGoogle Scholar,
while putrescine is born from L-carnitine or L-arginine A Trusted Source Michael AJ. Biosynthesis of polyamines and polyamine-containing molecules.Biochem J(2016) 473:2315–29. doi: 10.1042/BCJ20160185 PubMed AbstractCrossRef Full TextGoogle Scholar.
Spermidine, a bit more complex, is derived from S-adenosine-L-methionine and putrescine A Trusted Source Tabor CW, Tabor H. The speEspeD operon of Escherichia coli. Formation and processing of a proenzyme form of S-adenosylmethionine decarboxylase.J Biol Chem(1987) 262:16037–40. doi: 10.1016/S0021-9258(18)47692-2 PubMed AbstractCrossRef Full TextGoogle Scholar.
These tiny molecules are more than just byproducts; they're part of a microscopic world that impacts our heart health A Trusted Source Ramos-Molina B, Queipo-Ortuno MI, Lambertos A, Tinahones FJ, Penafiel R. Dietary and gut microbiota polyamines in obesity- and age-related diseases.Front Nutr(2019) 6:24. doi: 10.3389/fnut.2019.00024 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Madeo F, Eisenberg T, Pietrocola F, Kroemer G. Spermidine in health and disease.Science(2018) 359(6374):eaan2788. doi: 10.1126/science.aan2788 PubMed AbstractCrossRef Full TextGoogle Scholar.
Researchers like Liu S. et al. have delved into spermidine's effects and found promising results.
In mice with abdominal aortic aneurysms, a condition tangled with gut bacteria imbalance, spermidine shifted the bacterial community to a friendlier, anti-inflammatory state A Trusted Source Liu S, Liu Y, Zhao J, Yang P, Wang W, Liao M. Effects of spermidine on gut microbiota modulation in experimental abdominal aortic aneurysm mice.Nutrients(2022) 14(16):3349. doi: 10.3390/nu14163349 PubMed AbstractCrossRef Full TextGoogle Scholar.
Not only does spermidine help foster beneficial bacteria, but it also boosts our gut's defense system A Trusted Source Liu S, Liu Y, Zhao J, Yang P, Wang W, Liao M. Effects of spermidine on gut microbiota modulation in experimental abdominal aortic aneurysm mice.Nutrients(2022) 14(16):3349. doi: 10.3390/nu14163349PubMed AbstractCrossRef Full TextGoogle Scholar.
When it comes to the heart, spermidine is like a multitasking superhero.
It combats heart enlargement and supports better heart function A Trusted Source Lagkouvardos I, Lesker TR, Hitch TCA, Galvez EJC, Smit N, Neuhaus K, et al. Sequence and cultivation study of Muribaculaceae reveals novel species, host preference, and functional potential of this yet undescribed family.Microbiome(2019) 7:28. doi: 10.1186/s40168-019-0637-2 PubMed AbstractCrossRef Full TextGoogle Scholar.
Plus, it orchestrates a gut environment that helps bacteria-producing anti-inflammatory substances thrive, nudging us toward a healthier life A Trusted Source Smith BJ, Miller RA, Schmidt TM. Muribaculaceae genomes assembled from metagenomes suggest genetic drivers of differential response to acarbose treatment in mice.mSphere(2021) 6:e0085121. doi: 10.1128/msphere.00851-21 PubMed AbstractCrossRef Full TextGoogle Scholar.
Although in large doses, cadaverine and putrescine could make us feel queasy A Trusted Source Omer AK, Mohammed RR, Ameen PSM, Abas ZA, Ekici K. Presence of biogenic amines in food and their public health implications: A review.J Food Prot(2021) 84:1539–48. doi: 10.4315/JFP-21-047 PubMed AbstractCrossRef Full TextGoogle Scholar, their interplay with our body is crucial.
Understanding these relationships could be the key to unlocking new strategies for a healthy heart.
Based on the article you provided, here is a discussion and conclusion:
Discussion
- The gut microbiota, including bacteria, fungi, viruses, and protozoa, has a significant impact on heart health by influencing metabolism, inflammation, and immune responses.
- Dysbiosis, an imbalance in gut bacteria, can lead to inflammation and immune system problems, contributing to conditions like gut disorders and heart disease.
- The ratio of Firmicutes to Bacteroidetes in the gut is considered an indicator of overall health.
- Gut bacteria produce metabolites like trimethylamine N-oxide (TMAO), which has been linked to an increased risk of heart disease.
- The virome, including viruses and phages, may serve as potential risk markers for heart issues.
- Certain fungi, such as Candida and Mucor spp., have been associated with cardiovascular diseases, but more research is needed to fully understand these connections.
Conclusion
Understanding the role of the gut microbiota in heart health is crucial for developing innovative treatments and prevention strategies for cardiovascular diseases.
Maintaining a balanced gut microbiota, consuming a heart-friendly diet, and adopting a healthy lifestyle are important steps in reducing the risk of heart disease.
Further research is needed to explore the complex interactions between gut bacteria, viruses, fungi, and heart health to unlock new strategies for promoting cardiovascular well-being.
Review date not set.
How we reviewed this article:
Latest on:





