Gut Microbiota Dysbiosis: A Silent Player in Neurological Disorders
Explore the connection between dysbiosis and neurological disorders in this informative blog post. Gain insights into the impact of gut microbiota on brain health.

Introduction
In the intricate symphony of human health, the gut microbiota plays a role often underestimated and frequently overlooked.
It is a vast and diverse ecosystem of microorganisms that inhabit our gastrointestinal tract, collectively known as the gut microbiota.
Over the years, mounting evidence has illuminated its multifaceted significance, extending far beyond digestion.
Recent scientific endeavors have unearthed an intriguing connection between the gut microbiota and neurological disorders, ushering in a new era of exploration into the gut-brain axis.
Amidst this revelation, one term has gained prominence - "Gut Microbiota Dysbiosis," signifying an imbalance within this microbial community.
In this journey through the intricate landscape of human biology, we embark on a quest to understand the silent yet impactful role of gut microbiota dysbiosis in neurological disorders.
This article delves into the realms of autism spectrum disorder (ASD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and schizophrenia, where the gut microbiota's composition becomes a critical player in the unfolding narratives of these conditions.
As we venture deeper, we'll explore the potential of prebiotics as a beacon of hope, offering a means to restore harmony within this microbial orchestra and potentially alleviate the burden of neurological disorders.
Join us as we unravel the mysteries of gut microbiota dysbiosis and discover the promising prospects that prebiotics hold in our ongoing quest for neurological wellness.
Back to TopThe Human Gut Microbiome: A Vital Organ
The human gut microbiome (GM) has long been recognized as crucial for human health, with its significance dating back to ancient times.
Hippocrates, a renowned figure in the history of medicine, made the profound statement, "Death sits in the bowels" in 400 B.C. A Trusted Source Hou, K.; Wu, Z.-X.; Chen, X.-Y.; Wang, J.-Q.; Zhang, D.; Xiao, C.; Zhu, D.; Koya, J.B.; Wei, L.; Li, J.; et al. Microbiota in health and diseases. Signal Transduct. Target. Ther. 2022, 7, 135. [Google Scholar] [CrossRef]A Complex Ecosystem in Your Gut
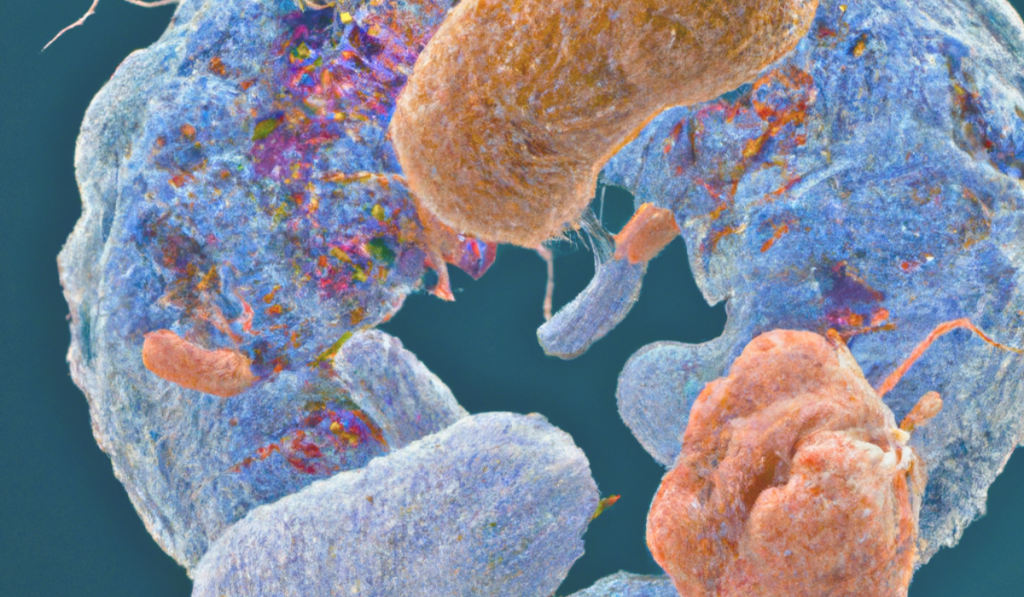
The GM is an intricate and dynamic ecosystem that resides in your gastrointestinal tract (GIT), comprising a diverse community of bacteria, viruses, fungi, and protozoa. A Trusted Source Afzaal, M.; Saeed, F.; Shah, Y.A.; Hussain, M.; Rabail, R.; Socol, C.T.; Hassoun, A.; Pateiro, M.; Lorenzo, J.M.; Rusu, A.V. Human gut microbiota in health and disease: Unveiling the relationship. Front. Microbiol. 2022, 13, 999001. [Google Scholar] Surprisingly, the number of microbial cells in your body nearly matches the number of human cells. A Trusted Source Sender, R.; Fuchs, S.; Milo, R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016, 14, e1002533. [Google Scholar] The caecum and proximal colon house the highest microbial biomass. A Trusted Source Matzaras, R.; Nikopoulou, A.; Protonotariou, E.; Christaki, E. Gut microbiota modulation and prevention of dysbiosis as an alternative approach to antimicrobial resistance: A narrative review. Yale J. Biol. Med. 2022, 95, 479. [Google Scholar] Your GM is influenced by various factors, including genetics, diet, environment, lifestyle, early microbial exposure, and the immune system. A Trusted Source Matzaras, R.; Nikopoulou, A.; Protonotariou, E.; Christaki, E. Gut microbiota modulation and prevention of dysbiosis as an alternative approach to antimicrobial resistance: A narrative review. Yale J. Biol. Med. 2022, 95, 479. [Google Scholar] Although individual GM profiles vary at the species and genus level, there is consistency in the distribution of major phyla throughout the intestine among healthy individuals. A Trusted Source Carabotti, M.; Scirocco, A.; Maselli, M.A.; Severi, C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. Q. Publ. Hell. Soc. Gastroenterol. 2015, 28, 203. [Google Scholar] The dominant phyla in the adult gut include Firmicutes, Bacteroidetes, Actinobacteria, Proteobacteria, Fusobacteria, Verrucomicrobia, and Cyanobacteria. A Trusted Source Van de Wouw, M.; Schellekens, H.; Dinan, T.G.; Cryan, J.F. Microbiota-gut-brain axis: Modulator of host metabolism and appetite. J. Nutr. 2017, 147, 727–745. [Google Scholar] [CrossRef] Additionally, the GM contains fungi, viruses, phages, and archaea, all playing essential roles. A Trusted Source Auchtung, T.A.; Fofanova, T.Y.; Stewart, C.J.; Nash, A.K.; Wong, M.C.; Gesell, J.R.; Auchtung, J.M.; Ajami, N.J.; Petrosino, J.F. Investigating colonization of the healthy adult gastrointestinal tract by fungi. MSphere 2018, 3, e00092-18. [Google Scholar] [CrossRef] A Trusted Source Matijašić, M.; Meštrović, T.; Čipčić Paljetak, H.; Perić, M.; Barešić, A.; Verbanac, D. Gut microbiota beyond bacteria—Mycobiome, virome, archaeome, and eukaryotic parasites in IBD. Int. J. Mol. Sci. 2020, 21, 2668. [Google Scholar]Your Gut Microbiome and You
The GM doesn't just coexist with you; it plays a central role in maintaining your body's balance and influencing various physiological functions.
It impacts metabolism, synthesizes vitamins, maintains barriers against pathogens, shapes your immune system, contributes to hematopoiesis, and even affects your behavior. A Trusted Source Afzaal, M.; Saeed, F.; Shah, Y.A.; Hussain, M.; Rabail, R.; Socol, C.T.; Hassoun, A.; Pateiro, M.; Lorenzo, J.M.; Rusu, A.V. Human gut microbiota in health and disease: Unveiling the relationship. Front. Microbiol. 2022, 13, 999001. [Google Scholar] A Trusted Source Ahlawat, S.; Asha; Sharma, K. Gut–organ axis: A microbial outreach and networking. Lett. Appl. Microbiol. 2021, 72, 636–668. [Google Scholar] Recent research highlights the "gut-organ axis," revealing bidirectional interactions between the GM and other organs. A Trusted Source Guo, Y.; Chen, X.; Gong, P.; Li, G.; Yao, W.; Yang, W. The Gut–Organ-Axis Concept: Advances the Application of Gut-on-Chip Technology. Int. J. Mol. Sci. 2023, 24, 4089. [Google Scholar]This communication is facilitated by signaling pathways and chemical interactions between the host and microorganisms.
Microbial Dysbiosis: When Things Go Wrong
Any deviation from a healthy GM composition is termed "microbial dysbiosis."
This imbalance can manifest in several ways, including the loss of beneficial microorganisms, the presence of harmful microorganisms, or a reduction in overall microbial diversity. A Trusted Source Petersen, C.; Round, J.L. Defining dysbiosis and its influence on host immunity and disease. Cell. Microbiol. 2014, 16, 1024–1033. [Google Scholar] [PubMed] Various factors, such as genetics, diet, disease, and stress, can disrupt GM homeostasis. A Trusted Source Das, B.; Nair, G.B. Homeostasis and dysbiosis of the gut microbiome in health and disease. J. Biosci. 2019, 44, 117. [Google Scholar]Dysbiosis has been linked to conditions like inflammatory bowel disease (IBD), malnutrition, metabolic disorders, asthma, and neurodegenerative diseases.
However, it's not always clear whether the altered GM causes these diseases or merely reflects their presence.
Harnessing the Power of Prebiotics
Researchers are exploring ways to restore the GM in various diseases, and one promising avenue is through the use of prebiotics.
Prebiotics are substances that selectively promote the growth of beneficial microorganisms in your gut, conferring health benefits. A Trusted Source Ng, Q.X.; Loke, W.; Venkatanarayanan, N.; Lim, D.Y.; Soh, A.Y.S.; Yeo, W.S. A systematic review of the role of prebiotics and probiotics in autism spectrum disorders. Medicina 2019, 55, 129. [Google Scholar] [PubMed] Well-known prebiotics include fructo-oligosaccharides (FOS), galacto-oligosaccharides (GOS), lactulose, and inulin. A Trusted Source Saxami, G.; Mitsou, E.K.; Kerezoudi, E.N.; Mavrouli, I.; Vlassopoulou, M.; Koutrotsios, G.; Mountzouris, K.C.; Zervakis, G.I.; Kyriacou, A. In Vitro Fermentation of Edible Mushrooms: Effects on Faecal Microbiota Characteristics of Autistic and Neurotypical Children. Microorganisms 2023, 11, 414. [Google Scholar]Some studies even suggest that certain mushroom-derived β-glucans can serve as prebiotics.
Additionally, whole-food-based treatments are being investigated for their potential to modulate the GM through synergistic interactions between food components.
HIGHLIGHT
The human gut microbiome (GM) is a vital, complex ecosystem influencing health. Dysbiosis links to diseases, while prebiotics offer the potential for restoration.
Back to TopThe Fascinating Gut-Brain Axis: Exploring Bidirectional Communication
The gut-brain axis is an intricate system that allows for communication between our gut and our nervous system.
It's a remarkable phenomenon with implications for our well-being.
Here, we'll delve into this captivating subject.
The gut-brain axis is like a two-way street that lets our gut and our brain talk to each other. A Trusted Source Sandhu, K.V.; Sherwin, E.; Schellekens, H.; Stanton, C.; Dinan, T.G.; Cryan, J.F. Feeding the microbiota-gut-brain axis: Diet, microbiome, and neuropsychiatry. Transl. Res. 2017, 179, 223–244. [Google Scholar] But how does it work? Imagine this: your gut, known as the gastrointestinal microbiome (GM), can send messages that influence how your brain functions. A Trusted Source Naveed, M.; Zhou, Q.-G.; Xu, C.; Taleb, A.; Meng, F.; Ahmed, B.; Zhang, Y.; Fukunaga, K.; Han, F. Gut-brain axis: A matter of concern in neuropsychiatric disorders…! Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 104, 110051. [Google Scholar] It's almost like your gut has a direct line to your brain!Not to be outdone, your brain can send signals that affect what's happening in your gut.
Think of it as your brain giving orders to your gut.
This communication involves various components, like the central nervous system (CNS), parts of the gut's own nervous system (ENS), and the autonomic nervous system (ANS). A Trusted Source Saxami, G.; Mitsou, E.K.; Kerezoudi, E.N.; Mavrouli, I.; Vlassopoulou, M.; Koutrotsios, G.; Mountzouris, K.C.; Zervakis, G.I.; Kyriacou, A. In Vitro Fermentation of Edible Mushrooms: Effects on Faecal Microbiota Characteristics of Autistic and Neurotypical Children. Microorganisms 2023, 11, 414. [Google Scholar]It's a team effort!
The hypothalamic-pituitary-adrenal axis (HPA) is the stress efferent axis in your body. A Trusted Source Carabotti, M.; Scirocco, A.; Maselli, M.A.; Severi, C. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. Q. Publ. Hell. Soc. Gastroenterol. 2015, 28, 203. [Google Scholar]When stress or inflammation is around, it starts a chain reaction that involves hormones like cortisol.
Your brain has a say in how your gut behaves too. A Trusted Source Breit, S.; Kupferberg, A.; Rogler, G.; Hasler, G. Vagus nerve as modulator of the brain–gut axis in psychiatric and inflammatory disorders. Front. Psychiatry 2018, 9, 44. [Google Scholar] [PubMed] It can influence immune cells, epithelial cells, and enteric neurons. Surprisingly, your gut microbiome can have its say in all of this. A Trusted Source Miri, S.; Yeo, J.; Abubaker, S.; Hammami, R. Neuromicrobiology, an emerging neurometabolic facet of the gut microbiome? Front. Microbiol. 2023, 14, 1098412. [Google Scholar]It can influence your body's central processes, both directly and indirectly.
Sometimes, changes in the gut's permeability can have far-reaching effects. A Trusted Source Yarandi, S.S.; Peterson, D.A.; Treisman, G.J.; Moran, T.H.; Pasricha, P.J. Modulatory effects of gut microbiota on the central nervous system: How gut could play a role in neuropsychiatric health and diseases. J. Neurogastroenterol. Motil. 2016, 22, 201. [Google Scholar]This might involve factors like lipopolysaccharides (LPS).
The vagus nerve is like a direct phone line between your gut and your brain. A Trusted Source Yarandi, S.S.; Peterson, D.A.; Treisman, G.J.; Moran, T.H.; Pasricha, P.J. Modulatory effects of gut microbiota on the central nervous system: How gut could play a role in neuropsychiatric health and diseases. J. Neurogastroenterol. Motil. 2016, 22, 201. [Google Scholar]It plays a big role in things like hunger, stress, and inflammation.
The gut-brain axis isn't just about digestion. It can affect your mood, motivation, and even higher-level thinking.
But beware! When the balance between your body and gut bacteria gets disrupted, trouble can follow.
Researchers link this to various health problems.
HIGHLIGHT
The gut-brain axis facilitates bidirectional communication between the gut and brain, influencing various bodily functions, including stress responses, immune activity, and mood, with significant health implications.
This table provides a comprehensive overview of dysbiotic events observed in the GM of individuals affected by these neurodegenerative diseases.
| Neurodegenerative Disease | Main Dysbiotic Events in GM |
|---|---|
| Autism Spectrum Disorder (ASD) | - Higher abundances of Bacteroides, Parabacteroides, Clostridium, Faecalibacterium, and Phascolarctobacterium and a lower relative abundance of Streptococcus and Bifidobacterium in ASD patients - Dysbiosis in ASD children may influence the development and severity of ASD symptomatology |
| Parkinson's Disease (PD) | - Enrichment of the genera Lactobacillus, Akkermansia, and Bifidobacterium and depletion of bacteria belonging to the Lachnospiraceae family and the Faecalibacterium genus in PD patients |
| Amyotrophic Lateral Sclerosis (ALS) | - Reduced ratio of Firmicutes/Bacteroidetes, decreased abundance of butyrate -producing Oscillibacter, Anaerostipes, Lachnospira counts, and Prevotella, increased abundance of glucose-metabolizing Dorea in ALS patients - GM composition alters during the course of the ALS |
| Schizophrenia | - In the schizophrenia group, an enhanced count of bacterial families like Prevotellaceae, Veillonellaceae, Bacteroidaceae, and Coriobacteriaceae was observed compared to healthy controls, while Ruminococcus and Roseburia abundances were significantly lower in patients with schizophrenia - Specific bacteria may function as biomarkers to differentiate schizophrenia from healthy individuals - Differences in GM between remission and acute schizophrenia as well as between first-episode drug-naïve and chronically medicated schizophrenia patients |
Each entry in the table summarizes key dysbiotic events associated with a specific neurodegenerative disease, supported by relevant scientific references.
The information presented here contributes to the growing body of knowledge surrounding the gut-brain axis and its role in neurodegenerative conditions
Gut Dysbiosis in Neurologic Diseases
Our gut is home to a vast community of microorganisms known as the gut microbiota (GM).
When these microorganisms become imbalanced, a condition referred to as "dysbiosis," it can have significant implications for our health, including our brain. A Trusted Source Intili, G.; Paladino, L.; Rappa, F.; Alberti, G.; Plicato, A.; Calabrò, F.; Fucarino, A.; Cappello, F.; Bucchieri, F.; Tomasello, G. From Dysbiosis to Neurodegenerative Diseases through Different Communication Pathways: An Overview. Biology 2023, 12, 195. [Google Scholar]Dysbiosis can trigger inflammation, both in the gut and throughout the body, affecting the integrity of the gut's protective barrier.
This disruption allows substances like hormones and microbial byproducts to enter the bloodstream.
Remarkably, some of these substances can travel to the brain through the vagus nerve, even bypassing the protective blood-brain barrier.
This process can initiate neurodegenerative processes that affect brain health.
Furthermore, dysbiosis can make the brain's cells more permeable, potentially leading to neuroinflammation and issues with nerve cells.
Emerging research indicates that gut dysbiosis may play a role in the development and progression of various neurological disorders, such as autism spectrum disorder (ASD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and schizophrenia. A Trusted Source Intili, G.; Paladino, L.; Rappa, F.; Alberti, G.; Plicato, A.; Calabrò, F.; Fucarino, A.; Cappello, F.; Bucchieri, F.; Tomasello, G. From Dysbiosis to Neurodegenerative Diseases through Different Communication Pathways: An Overview. Biology 2023, 12, 195. [Google Scholar]Understanding the intricate connection between gut health and brain health is crucial, as it may offer valuable insights into preventing and treating neurological disorders.

Dysbiosis in Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is a group of complex neurodevelopmental disorders characterized by atypical social interactions, communication difficulties, repetitive behaviors, and unusual sensory responses. A Trusted Source Zhu, J.; Guo, M.; Yang, T.; Lai, X.; Tang, T.; Chen, J.; Li, L.; Li, T. Nutritional Status and Symptoms in Preschool Children With Autism Spectrum Disorder: A Two-Center Comparative Study in Chongqing and Hainan Province, China. Front. Pediatr. 2020, 8, 469. [Google Scholar] [PubMed] Recent research has shed light on the prevalence of ASD, with a rate of 1.70% among 4-year-old children and 1.85% among 8-year-olds in the United States, while in Europe, it varies between 0.38% and 1.55%. A Trusted Source Bougeard, C.; Picarel-Blanchot, F.; Schmid, R.; Campbell, R.; Buitelaar, J. Prevalence of Autism Spectrum Disorder and Co-morbidities in Children and Adolescents: A Systematic Literature Review. Front. Psychiatry 2021, 12, 744709. [Google Scholar] [PubMed]
The exact cause of ASD is still unclear, but both genetic and environmental factors are believed to play a role.
Recent studies have started to explore the connection between the gut and the brain, known as the gut-brain axis, in various neuropsychiatric conditions, including ASD.
Additionally, many individuals with ASD often experience gastrointestinal issues like constipation, diarrhea, bloating, increased gut permeability, and abdominal pain. A Trusted Source Andreo-Martínez, P.; García-Martínez, N.; Sánchez-Samper, E.; González, A. An approach to gut microbiota profile in children with autism spectrum disorder. Environ. Microbiol. Rep. 2019, 12, 115–135. [Google Scholar] [CrossRef] A Trusted Source Yitik Tonkaz, G.; Esin, I.S.; Turan, B.; Uslu, H.; Dursun, O.B. Determinants of Leaky Gut and Gut Microbiota Differences in Children With Autism Spectrum Disorder and Their Siblings. J. Autism Dev. Disord. 2022, 53, 2703–2716. [Google Scholar] [CrossRef]One interesting area of research is the composition of the gut microbiota (GM) in ASD.
While specific microbial species have not been consistently identified as differentiating ASD from neurotypical children, factors like diet, age, sex, population, and the severity of autism need to be considered. A Trusted Source Alharthi, A.; Alhazmi, S.; Alburae, N.; Bahieldin, A. The Human Gut Microbiome as a Potential Factor in Autism Spectrum Disorder. Int. J. Mol. Sci. 2022, 23, 1363. [Google Scholar] [CrossRef] [PubMed] Nevertheless, autistic children often exhibit microbial imbalances, including higher levels of Bacteroides, Parabacteroides, Clostridium, Faecalibacterium, and Phascolarctobacterium, and lower levels of Streptococcus and Bifidobacterium. A Trusted Source Andreo-Martínez, P.; García-Martínez, N.; Sánchez-Samper, E.; González, A. An approach to gut microbiota profile in children with autism spectrum disorder. Environ. Microbiol. Rep. 2019, 12, 115–135. [Google Scholar] [CrossRef] A Trusted Source Iglesias-Vázquez, L.; Van Ginkel Riba, G.; Arija, V.; Canals, J. Composition of Gut Microbiota in Children with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 792. [Google Scholar] [CrossRef] In recent studies, it was observed that neurotypical children had higher levels of Prevotella spp. and Bifidobacterium spp. compared to children with ASD. A Trusted Source Saxami, G.; Mitsou, E.K.; Kerezoudi, E.N.; Mavrouli, I.; Vlassopoulou, M.; Koutrotsios, G.; Mountzouris, K.C.; Zervakis, G.I.; Kyriacou, A. In Vitro Fermentation of Edible Mushrooms: Effects on Faecal Microbiota Characteristics of Autistic and Neurotypical Children. Microorganisms 2023, 11, 414. [Google Scholar]Another study found differences in the GM structure between ASD and healthy control groups, with higher levels of unidentified Lachnospiraceae, Clostridiales, Erysipelotrichaceae, Dorea, Collinsella, and Lachnoclostridium strains in the ASD group and lower levels of Bacteroides, Faecalibacterium, Parasutterella, and Paraprevotella.
Remarkably, the composition of the GM was linked to the severity of autism symptoms, suggesting that regulating the gut microbiota might be a potential strategy for future ASD treatments A Trusted Source Ding, X.; Xu, Y.; Zhang, X.; Zhang, L.; Duan, G.; Song, C.; Li, Z.; Yang, Y.; Wang, Y.; Wang, X. Gut microbiota changes in patients with autism spectrum disorders. J. Psychiatr. Res. 2020, 129, 149–159. [Google Scholar]Furthermore, there appears to be a significant correlation between gastrointestinal symptoms and behavioral and cognitive challenges in individuals with ASD.
Symptoms such as irritability, aggression, sleep disturbances, and self-injury are often linked to GI issues. A Trusted Source Andreo-Martínez, P.; García-Martínez, N.; Sánchez-Samper, E.; González, A. An approach to gut microbiota profile in children with autism spectrum disorder. Environ. Microbiol. Rep. 2019, 12, 115–135. [Google Scholar] [CrossRef] A Trusted Source Chakraborty, P.; Carpenter, K.L.H.; Major, S.; Deaver, M.; Vermeer, S.; Herold, B.; Franz, L.; Howard, J.; Dawson, G. Gastrointestinal problems are associated with increased repetitive behaviors but not social communication difficulties in young children with autism spectrum disorders. Autism 2021, 25, 405–415. [Google Scholar] [CrossRef] This evidence points to a potential link between gastrointestinal problems, possibly connected to gut dysbiosis (microbial imbalances), and ASD. A Trusted Source Cryan, J.F.; Dinan, T.G. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012, 13, 701–712. [Google Scholar] [CrossRef] A meta-analysis even suggested that dysbiosis in children with ASD might influence the development and severity of their symptoms, with the microbiota predominantly composed of the phyla Bacteroidetes, Firmicutes, and Actinobacteria, along with higher levels of Bacteroides, Parabacteroides, Clostridium, Faecalibacterium, and Phascolarctobacterium, and lower levels of Coprococcus and Bifidobacterium. A Trusted Source Iglesias-Vázquez, L.; Van Ginkel Riba, G.; Arija, V.; Canals, J. Composition of Gut Microbiota in Children with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 792. [Google Scholar] [CrossRef]HIGHLIGHT
Autism Spectrum Disorder (ASD) involves complex neurodevelopmental issues. Recent research explores gut-brain links, microbiota variations, and their potential impact on ASD symptoms and future treatment possibilities
Dysbiosis in Parkinson’s Disease
Parkinson's Disease (PD) ranks as the second most common neurodegenerative brain disorder, impacting an estimated seven to ten million people worldwide. A Trusted Source Faruqui, N.A.; Prium, D.H.; Mowna, S.A.; Rahaman, T.I.; Dutta, A.R.; Akter, M.F. Identification of Common Molecular Signatures Shared between Alzheimer’s and Parkinson’s Diseases and Therapeutic Agents Exploration: An Integrated Genomics Approach. bioRxiv 2021. [Google Scholar] [CrossRef]
This complex condition is characterized by a range of motor and non-motor symptoms that significantly affect a person's quality of life.
Motor symptoms include resting tremors, muscle stiffness, slowed movements, and difficulties with walking.
In addition, PD can bring cognitive challenges, depression, mood swings, altered senses, and disrupted sleep patterns. A Trusted Source Ma, Q.; Xing, C.; Long, W.; Wang, H.Y.; Liu, Q.; Wang, R.-F. Impact of microbiota on central nervous system and neurological diseases: The gut-brain axis. J. Neuroinflammation 2019, 16, 53. [Google Scholar] [PubMed]The central issue in PD lies in a specific brain region called the substantia nigra, where dopamine-producing neurons gradually diminish.
Concurrently, an abnormal protein called alpha-synuclein (alpha-syn) accumulates, forming structures known as Lewy bodies and Lewy neurites—a condition referred to as synucleinopathy. A Trusted Source Stopińska, K.; Radziwoń-Zaleska, M.; Domitrz, I. The Microbiota-Gut-Brain Axis as a Key to Neuropsychiatric Disorders: A Mini Review. J. Clin. Med. 2021, 10, 4640. [Google Scholar] [CrossRef]While the exact causes of PD remain elusive, a combination of genetic and environmental factors is known to contribute.
Gastrointestinal issues are also prevalent among PD patients, encompassing symptoms like excessive salivation, swallowing difficulties, constipation, nausea, irregular bowel movements, and defecation problems.
Recent research has uncovered intriguing changes in the gut microbiome (GM) of PD patients. A Trusted Source Elfil, M.; Kamel, S.; Kandil, M.; Koo, B.B.; Schaefer, S.M. Implications of the gut microbiome in Parkinson’s disease. Mov. Disord. 2020, 35, 921–933. [Google Scholar] A Trusted Source Grochowska, M.; Laskus, T.; Radkowski, M. Gut microbiota in neurological disorders. Arch. Immunol. Ther. Exp. 2019, 67, 375–383. [Google Scholar] A Trusted Source Lin, A.; Zheng, W.; He, Y.; Tang, W.; Wei, X.; He, R.; Huang, W.; Su, Y.; Huang, Y.; Zhou, H.; et al. Gut microbiota in patients with Parkinson’s disease in southern China. Park. Relat. Disord. 2018, 53, 82–88. [Google Scholar] [CrossRef] A comprehensive meta-analysis by Romano and colleagues reanalyzed ten existing 16S microbiome datasets and identified significant alterations in the microbiome associated with PD. A Trusted Source Romano, S.; Savva, G.; Bedarf, J.; Charles, I.; Hildebrand, F.; Narbad, A. Meta-analysis of the Parkinson’s disease gut microbiome suggests alterations linked to intestinal inflammation. npj Park. Dis. 2021, 7, 27. [Google Scholar] [CrossRef]Specifically, the analysis showed an increase in bacteria from the Lactobacillus, Akkermansia, and Bifidobacterium genera, alongside a decrease in bacteria from the Lachnospiraceae family and the Faecalibacterium genus.
These changes suggest a state of dysbiosis, potentially linked to inflammation, which could contribute to the gastrointestinal symptoms seen in PD.
Another study revealed increased levels of Verrucomicrobiaceae at the family level, the Akkermansia genus, and the Akkermansia muciniphila species, while beneficial bacteria like Roseburia and Faecalibaterium, which produce butyrate (a beneficial compound), were found to decrease in PD patients. A Trusted Source Guo, T.; Chen, L. Gut microbiota and inflammation in Parkinson’s disease: Pathogenetic and therapeutic insights. Eur. J. Inflamm. 2022, 20, 1721727X221083763. [Google Scholar] [CrossRef] Emerging research also indicates connections between GM changes and various PD symptoms, including both motor and non-motor aspects. A Trusted Source Vascellari, S.; Melis, M.; Palmas, V.; Pisanu, S.; Serra, A.; Perra, D.; Santoru, M.L.; Oppo, V.; Cusano, R.; Uva, P. Clinical phenotypes of Parkinson’s disease associate with distinct gut microbiota and metabolome enterotypes. Biomolecules 2021, 11, 144. [Google Scholar]The disruption in the GM could be a crucial factor.
Several studies support the hypothesis that GM dysbiosis in PD is associated with increased permeability of the intestinal barrier, leading to gut inflammation.
This inflammation is a recognized symptom in PD patients. A Trusted Source Yang, D.; Zhao, D.; Ali Shah, S.Z.; Wu, W.; Lai, M.; Zhang, X.; Li, J.; Guan, Z.; Zhao, H.; Li, W. The role of the gut microbiota in the pathogenesis of Parkinson’s disease. Front. Neurol. 2019, 10, 1155. [Google Scholar]HIGHLIGHT
Parkinson's Disease (PD), affecting 7-10 million globally, exhibits motor and non-motor symptoms, linked to gut microbiome changes. GM dysbiosis may influence PD symptoms via gut inflammation
Back to TopThe Dysbiosis and Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS), a debilitating neurodegenerative disease, is characterized by the gradual loss of motor neurons in the brain's cortex, brain stem, and spinal cord.
This loss leads to muscle weakness and wasting. A Trusted Source Boddy, S.L.; Giovannelli, I.; Sassani, M.; Cooper-Knock, J.; Snyder, M.P.; Segal, E.; Elinav, E.; Barker, L.A.; Shaw, P.J.; McDermott, C.J. The gut microbiome: A key player in the complexity of amyotrophic lateral sclerosis (ALS). BMC Med. 2021, 19, 13. [Google Scholar] A Trusted Source Gotkine, M.; Kviatcovsky, D.; Elinav, E. Amyotrophic lateral sclerosis and intestinal microbiota—Toward establishing cause and effect. Gut Microbes 2020, 11, 1833–1841. [Google Scholar] In addition to motor symptoms, ALS also involves cognitive and behavioral disturbances. A Trusted Source McCombe, P.A.; Henderson, R.D.; Lee, A.; Lee, J.D.; Woodruff, T.M.; Restuadi, R.; McRae, A.; Wray, N.R.; Ngo, S.; Steyn, F.J. Gut microbiota in ALS: Possible role in pathogenesis? Expert Rev. Neurother. 2019, 19, 785–805. [Google Scholar]Over 90% of ALS cases are sporadic (sALS), with no known cause, while the remaining 10% are familial (fALS) and are linked to specific genetic mutations.
Mutations in genes such as superoxide dismutase 1 (SOD1), FUS RNA binding protein (FUS/TLS), C9orf72-SMCR8 complex subunit (C9orf72), and TAR DNA binding protein (TARDBP/TDP-43) are commonly associated with ALS. A Trusted Source Zeng, Q.; Shen, J.; Chen, K.; Zhou, J.; Liao, Q.; Lu, K.; Yuan, J.; Bi, F. The alteration of gut microbiome and metabolism in amyotrophic lateral sclerosis patients. Sci. Rep. 2020, 10, 12998. [Google Scholar] Despite extensive research efforts, the exact causes of ALS remain elusive, and currently, there is no cure available, often leading to respiratory failure and death within 2 to 5 years from the onset of symptoms. A Trusted Source Maskovic, J.; Ilic, A.; Zugic, V.; Stevic, Z.; Stjepanovic, M.I. What is the right moment for noninvasive ventilation in amyotrophic lateral sclerosis? Arch. Med. Sci. 2023, 19, 337. [Google Scholar] Recent studies have shed light on a significant connection between the gut microbiome (GM) and ALS. A Trusted Source Chidambaram, S.B.; Essa, M.M.; Rathipriya, A.; Bishir, M.; Ray, B.; Mahalakshmi, A.M.; Tousif, A.; Sakharkar, M.K.; Kashyap, R.S.; Friedland, R.P. Gut dysbiosis, defective autophagy and altered immune responses in neurodegenerative diseases: Tales of a vicious cycle. Pharmacol. Ther. 2022, 231, 107988. [Google Scholar]ALS pathogenesis appears to be influenced by changes in GM composition, metabolic disruptions, altered immune responses, and the production of neurotoxins by certain gut bacteria, such as Clostridia species, which can harm the brain.
However, the results of human studies investigating the role of GM in ALS have been inconclusive due to factors like small sample sizes, variability within the study populations, diverse experimental methods, and the natural variability of GM among individuals regardless of their health status.
Despite these challenges, some key findings have emerged:
Differences in GM populations between ALS patients and healthy individuals: A Trusted Source Fang, X.; Wang, X.; Yang, S.; Meng, F.; Wang, X.; Wei, H.; Chen, T. Evaluation of the microbial diversity in amyotrophic lateral sclerosis using high-throughput sequencing. Front. Microbiol. 2016, 7, 1479. [Google Scholar] [CrossRef]ALS patients exhibit a reduced ratio of Firmicutes to Bacteroidetes in their gut.
There is a decreased presence of beneficial butyrate-producing bacteria like Oscillibacter, Anaerostipes, and Lachnospira in ALS patients.
Conversely, ALS patients have an increased abundance of Dorea, which metabolizes glucose.
Comparing the gut microbiome of ALS patients and their spouses, it was discovered that ALS patients had a more diverse and less abundant Prevotella spp.
This indicates that addressing Prevotella spp. deficiency and altering butyrate metabolism could potentially be a promising treatment for ALS. A Trusted Source Hertzberg, V.S.; Singh, H.; Fournier, C.N.; Moustafa, A.; Polak, M.; Kuelbs, C.A.; Torralba, M.G.; Tansey, M.G.; Nelson, K.E.; Glass, J.D. Gut microbiome differences between amyotrophic lateral sclerosis patients and spouse controls. Amyotroph. Lateral Scler. Front. Degener. 2022, 23, 91–99. [Google Scholar] Changes in GM composition during the course of ALS: A Trusted Source Di Gioia, D.; Bozzi Cionci, N.; Baffoni, L.; Amoruso, A.; Pane, M.; Mogna, L.; Gaggìa, F.; Lucenti, M.A.; Bersano, E.; Cantello, R. A prospective longitudinal study on the microbiota composition in amyotrophic lateral sclerosis. BMC Med. 2020, 18, 153. [Google Scholar]A study of 50 ALS patients and 50 matched controls revealed differences in GM composition between the two groups.
Importantly, the composition of the intestinal microbiota changed as the disease progressed, with a significant decrease in the number of operational taxonomy units observed during follow-up.
An imbalance between potentially protective microbial groups (e.g., Bacteroidetes) and those with potential neurotoxic or pro-inflammatory activity (e.g., Cyanobacteria) was noted.
These findings strongly suggest that the gut microbiome plays a role in ALS.
However, it remains a challenge to determine whether these GM changes are a cause, an exacerbating factor, or a consequence of the disease.
Further clinical research in humans is needed to pinpoint the exact role of GM in the development and progression of ALS.
HIGHLIGHT
ALS, a neurodegenerative disease, exhibits links to the gut microbiome. Studies show differences in microbial composition in ALS patients, suggesting its potential role in disease development, but more research is needed.
Dysbiosis in Schizophrenia

Understanding the intricate interaction between genetic and environmental processes throughout the neurodevelopmental trajectory in this condition remains a challenging puzzle yet to be fully deciphered.
In recent years, there has been growing interest in the connection between schizophrenia and the gut microbiome (GM). A Trusted Source Zheng, P.; Zeng, B.; Liu, M.; Chen, J.; Pan, J.; Han, Y.; Liu, Y.; Cheng, K.; Zhou, C.; Wang, H. The gut microbiome from patients with schizophrenia modulates the glutamate-glutamine-GABA cycle and schizophrenia-relevant behaviors in mice. Sci. Adv. 2019, 5, eaau8317. [Google Scholar]Key findings from existing research include:
(a) Patients with schizophrenia exhibit distinct alterations in their GM composition compared to healthy individuals A Trusted Source Gokulakrishnan, K.; Nikhil, J.; Viswanath, B.; Thirumoorthy, C.; Narasimhan, S.; Devarajan, B.; Joseph, E.; David, A.K.D.; Sharma, S.; Vasudevan, K. Comparison of gut microbiome profile in patients with schizophrenia and healthy controls-A plausible non-invasive biomarker? J. Psychiatr. Res. 2023, 162, 140–149. [Google Scholar] [PubMed]These changes are seen in both the diversity and composition of the GM.
For instance, the GM of schizophrenia patients may show increased counts of certain bacterial families like Prevotellaceae, Veillonellaceae, Bacteroidaceae, and Coriobacteriaceae, while the abundances of Ruminococcus and Roseburia are significantly lower.
(b) Specific bacteria within the GM may serve as biomarkers to differentiate individuals with schizophrenia from those without the condition A Trusted Source Shen, Y.; Xu, J.; Li, Z.; Huang, Y.; Yuan, Y.; Wang, J.; Zhang, M.; Hu, S.; Liang, Y. Analysis of gut microbiota diversity and auxiliary diagnosis as a biomarker in patients with schizophrenia: A cross-sectional study. Schizophr. Res. 2018, 197, 470–477. [Google Scholar]Researchers have identified 12 such biomarkers that can be used for diagnostic purposes.
These include bacteria at various taxonomic levels, from the class level down to the species level. A Trusted Source Pan, R.; Zhang, X.; Gao, J.; Yi, W.; Wei, Q.; Su, H. Analysis of the diversity of intestinal microbiome and its potential value as a biomarker in patients with schizophrenia: A cohort study. Psychiatry Res. 2020, 291, 113260. [Google Scholar] [PubMed] (c) Differences in the GM composition have been observed between individuals with acute schizophrenia symptoms and those in remission A Trusted Source Pan, R.; Zhang, X.; Gao, J.; Yi, W.; Wei, Q.; Su, H. Analysis of the diversity of intestinal microbiome and its potential value as a biomarker in patients with schizophrenia: A cohort study. Psychiatry Res. 2020, 291, 113260. [Google Scholar] [PubMed]This suggests that alterations in the gut microbiota might influence the prognosis of the disease and raise the possibility of using GM as a non-invasive diagnostic tool.
(d) Distinct differences exist in the GM between individuals with first-episode drug-naïve schizophrenia and those who have been chronically medicated with antipsychotic drugs. A Trusted Source Ma, X.; Asif, H.; Dai, L.; He, Y.; Zheng, W.; Wang, D.; Ren, H.; Tang, J.; Li, C.; Jin, K. Alteration of the gut microbiome in first-episode drug-naïve and chronic medicated schizophrenia correlate with regional brain volumes. J. Psychiatr. Res. 2020, 123, 136–144. [Google Scholar]Chronically medicated patients tend to have lower microbial richness and diversity compared to their drug-naïve counterparts and healthy individuals.
This suggests that the gut microbiome could play a role in the pathophysiology of schizophrenia by affecting specific brain structures.
(e) The gut-brain axis, a bidirectional communication system between the gut and the brain, has been implicated in the association between the GM and schizophrenia A Trusted Source Yang, C.; Lin, X.; Wang, X.; Liu, H.; Huang, J.; Wang, S. The schizophrenia and gut microbiota: A bibliometric and visual analysis. Front. Psychiatry 2022, 13, 1022472. [Google Scholar] [PubMed]This involves processes such as immune regulation, neurotransmitter synthesis, production of bioactive microbial metabolites, and tryptophan metabolism.
Transplanting GM from individuals with schizophrenia into germ-free recipient rodents can induce schizophrenia-like behaviors, highlighting the potential influence of GM on brain neurochemistry associated with the onset of schizophrenia. A Trusted Source Zheng, P.; Zeng, B.; Liu, M.; Chen, J.; Pan, J.; Han, Y.; Liu, Y.; Cheng, K.; Zhou, C.; Wang, H. The gut microbiome from patients with schizophrenia modulates the glutamate-glutamine-GABA cycle and schizophrenia-relevant behaviors in mice. Sci. Adv. 2019, 5, eaau8317. [Google Scholar]HIGHLIGHT
Schizophrenia, a complex neurodevelopmental disorder, is linked to the gut microbiome. Altered microbial composition, biomarker potential, and the gut-brain axis suggest significant connections in understanding and treating schizophrenia
The Role of Prebiotics in Neurological Diseases
These mechanisms include reducing inflammation in gut disorders, optimizing GM composition, and influencing the production of essential neurochemicals.
Notably, prebiotics might have an advantage over probiotics in this context, as they are more likely to survive the harsh gastrointestinal environment.
Neurological Conditions: Numerous clinical studies have explored the effects of probiotics and symbiotics on various neurological conditions. A Trusted Source Lee, S.H.; Ahmad, S.R.; Lim, Y.C.; Zulkipli, I.N. The use of probiotic therapy in metabolic and neurological diseases. Front. Nutr. 2022, 9, 887019. [Google Scholar] A Trusted Source Sharma, V.; Kaur, S. The Effect of Probiotic Intervention in Ameliorating the Altered Central Nervous System Functions in Neurological Disorders: A Review. Open Microbiol. J. 2020, 14, 18–29. [Google Scholar] A Trusted Source Babu, C.S.; Chethan, N.; Rao, B.S.; Bhat, A.; Bipul, R.; Tousif, A.; Mahadevan, M.; Sathiya, S.; Manivasagam, T.; Thenmozhi, A.J. Probiotics, prebiotics, and synbiotics on neurological disorders: Relevance to Huntington’s disease. In Food for Huntington’s Disease; Nova Science Publishers, Inc.: Hauppauge, NY, USA, 2018; pp. 105–140. [Google Scholar]However, the use of prebiotics as a novel approach to treat neurological diseases has received limited attention.
In particular, there is a dearth of clinical studies on prebiotic interventions for Amyotrophic Lateral Sclerosis (ALS). A Trusted Source Lee, S.H.; Ahmad, S.R.; Lim, Y.C.; Zulkipli, I.N. The use of probiotic therapy in metabolic and neurological diseases. Front. Nutr. 2022, 9, 887019. [Google Scholar] Autism Spectrum Disorder (ASD): One pioneering study investigated the impact of a prebiotic, specifically the B-GOS® mixture, on GM composition and metabolic activity in 30 autistic children. A Trusted Source Grimaldi, R.; Gibson, G.R.; Vulevic, J.; Giallourou, N.; Castro-Mejía, J.L.; Hansen, L.H.; Leigh Gibson, E.; Nielsen, D.S.; Costabile, A. A prebiotic intervention study in children with autism spectrum disorders (ASDs). Microbiome 2018, 6, 133. [Google Scholar] [CrossRef]The results indicated that B-GOS® led to significant changes in GM composition, particularly affecting bifidobacterial populations and other bacterial groups.
Additionally, another study observed an improvement in GM dysbiosis in children with ASD following dietary supplementation with partially hydrolyzed guar gum (PHGG). A Trusted Source Inoue, R.; Sakaue, Y.; Kawada, Y.; Tamaki, R.; Yasukawa, Z.; Ozeki, M.; Ueba, S.; Sawai, C.; Nonomura, K.; Tsukahara, T.; et al. Dietary supplementation with partially hydrolyzed guar gum helps improve constipation and gut dysbiosis symptoms and behavioral irritability in children with autism spectrum disorder. J. Clin. Biochem. Nutr. 2019, 64, 217–223. [Google Scholar] [CrossRef]Notably, prebiotic interventions were associated with a decrease in behavioral irritability in children with ASD.
Parkinson's Disease: Researchers conducted two studies examining the effects of prebiotic supplementation in Parkinson's disease (PD). One study utilized resistant starch (RS) as a prebiotic intervention and reported a reduction in non-motor symptoms and a stable GM in PD patients A Trusted Source Becker, A.; Schmartz, G.; Gröger, L.; Grammes, N.; Galata, V.; Philippeit, H.; Weiland, J.; Ludwig, N.; Meese, E.; Tierling, S.; et al. Effects of Resistant Starch on Symptoms, Fecal Markers and Gut Microbiota in Parkinson’s Disease—The RESISTA-PD Trial. Genom. Proteom. Bioinform. 2021, 20, 274–287. [Google Scholar] [CrossRef] In another study, a prebiotic-containing bar intervention led to favorable changes in the GM composition, with a reduction in pro-inflammatory bacteria and an increase in Short-Chain Fatty Acid (SCFA)-producing bacteria. A Trusted Source Hall, D.; Voigt-Zuwala, R.; Jungles, T.; Hamaker, B.; Engen, P.; Shaikh, M.; Raeisi, S.; Green, S.; Naqib, A.; Forsyth, C.; et al. An open label, non-randomized study assessing a prebiotic fiber intervention in a small cohort of Parkinson’s disease participants. Nat. Commun. 2023, 14, 926. [Google Scholar] [CrossRef] [PubMed]Moreover, prebiotic treatment was associated with an improvement in the Unified Parkinson's Disease Rating Scale.
Schizophrenia: A study investigated the impact of lactosucrose, a prebiotic preparation, on a female subject with schizophrenia. A Trusted Source Ido, Y.; Nagamine, T.; Okamura, T.; Tasaki, M.; Fukuo, K. Prebiotic lactosucrose may improve not only constipation but also psychotic symptoms of Schizophrenia. Int. Med. J. 2017, 24, 305–306. [Google Scholar]After three months of lactosucrose administration while maintaining her medication, the subject experienced an improvement in psychotic symptoms.
Additionally, there was a significant decrease in the abundance of Clostridium and an increased Bifidobacterium-to-Clostridium ratio.
While promising, the effects of prebiotic supplementation on neurological diseases warrant further investigation.
The existing studies provide valuable insights into the potential benefits of prebiotics in modulating the GM-Brain Axis, but more comprehensive and long-term human research is needed to establish conclusive evidence. A Trusted Source Lee, S.H.; Ahmad, S.R.; Lim, Y.C.; Zulkipli, I.N. The use of probiotic therapy in metabolic and neurological diseases. Front. Nutr. 2022, 9, 887019. [Google Scholar] A Trusted Source Liu, X.; Cao, S.; Zhang, X. Modulation of gut microbiota–brain axis by probiotics, prebiotics, and diet. J. Agric. Food Chem. 2015, 63, 7885–7895. [Google Scholar]These findings offer hope for future therapeutic approaches to neurological conditions, potentially improving the quality of life for affected individuals.
Back to TopDiscussion
- Gut Microbiota Dysbiosis in Neurological Disorders:
- Examination of gut dysbiosis in autism spectrum disorder (ASD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and schizophrenia.
- Variations in gut microbiota composition and their potential impact on these neurological conditions.
- Evidence of associations between gut dysbiosis and the severity of symptoms in these disorders.
- Role of the Gut-Brain Axis:
- Highlighting the intricate communication between the gut and the brain through the gut-brain axis.
- Discussion of mechanisms such as immune regulation, neurotransmitter synthesis, microbial metabolites, and tryptophan metabolism.
- Prebiotics as a Promising Intervention:
- Examination of the potential benefits of prebiotics in neurological disorders.
- Prebiotic-induced modulation of gut microbiota composition and metabolic activity.
- Notable findings from studies involving prebiotic interventions in ASD, PD, and schizophrenia.
- Challenges and Future Directions:
- Acknowledgment of the need for further human clinical research to establish conclusive evidence.
- Addressing the complexities of gut microbiota research, including factors like sample size, population heterogeneity, and study design.
- Calls for continued investigation into the exact mechanisms through which gut dysbiosis contributes to neurological disorders.
Conclusion
- Gut microbiota dysbiosis emerges as a significant factor in various neurological disorders.
- Evidence suggests that alterations in gut microbiota composition are associated with disease severity and symptomatology.
- Prebiotics present a promising avenue for addressing gut dysbiosis and potentially alleviating symptoms in these conditions.
- While preliminary research is encouraging, additional comprehensive and long-term human studies are needed to confirm the therapeutic potential of prebiotics.
- This article underscores the critical importance of understanding and targeting the gut-brain axis to improve the management and treatment of neurological disorders.
Review date not set.
How we reviewed this article:
Latest on:





