Gut Bacteria: Orchestrating an Uplifting Gut-Brain Symphony
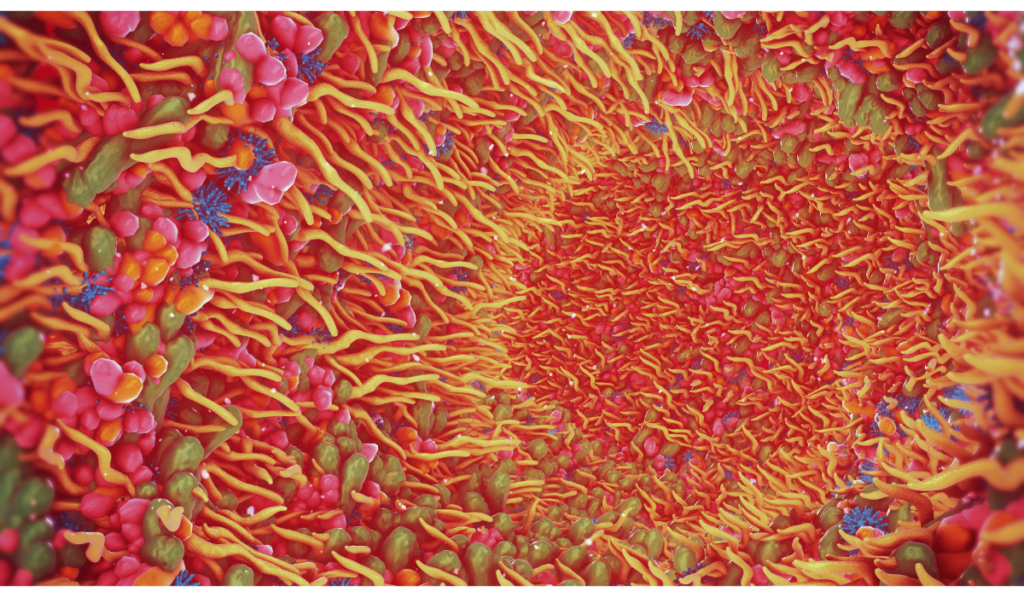
Explore the intricate connection between gut bacteria and the brain through the gut-brain axis. Unveil the impact of the gut microbiota on your overall well-being

In this article, we delve into the captivating link between the gut bacteria and the brain.
This exploration uncovers the hidden influences of neurotransmitters and microbes, shedding light on how they shape our health and emotions.
Welcome to a world where gut feelings take center stage.
Key Takeaways
- The communication between the brain, gut, and gut-to-brain pathways is increasingly recognized as crucial, with neurotransmitter 5-HT (serotonin) playing a significant role in this communication.
- Specific bacteria in the human and mouse gut can influence 5-HT levels in the gut and bloodstream, impacting gut-related disorders.
- Some psychotropic drugs, like SSRIs, can affect gut bacteria, suggesting a bidirectional influence between medication and the gut microbiota.
- Gut bacteria have been found to influence the development and proper functioning of the adult nervous system through 5-HT4 receptors.
- The gut microbiota can affect brain function by altering the levels of tryptophan, which is involved in serotonin production.
- Dysbiosis (imbalanced gut bacteria) may be associated with Irritable Bowel Syndrome (IBS) symptoms, but the exact relationship is still not fully understood.
- There is evidence suggesting a link between gut microbiota composition and mental health, particularly in cases of Major Depressive Disorder (MDD).
- Probiotics and dietary changes have shown potential benefits in managing IBS and mood disorders, but more research is needed to establish their effectiveness.
- Fecal microbiota transplantation (FMT) has shown promise in altering gut bacteria and improving IBS symptoms in some cases, but results can vary.
- The Microbiome-Gut-Brain (MGB) axis is an area of active research, revealing strong connections between gut health and brain function.
- Gender differences may exist in how gut bacteria affect brain development and susceptibility to stress-related disorders.
In This Article:
Mechanisms of Gut Microbiota to Gut-Brain Signaling
The Vagus Nerve: A Key Player in the Gut-Brain Axis
The vagus nerve is like a two-way highway between the brain and the gut. Scientists have done a lot of research on how this connection affects our health.
Although the sensory vagus nerve and digestive system are very connected, we still don't understand all the details of how they work together. Fulling C. Dinan T.G. Cryan J.F. Gut microbe to brain signaling: what happens in vagus. Neuron. 2019; 101: 998-1002 Scopus (84) PubMed Abstract Full Text Full Text PDF Google ScholarThe afferent branch of the vagus nerve is the main nerve connection between the gut and the brain that helps regulate emotions.
Although it does not directly interact with the gut microbiome, research suggests the vagus nerve can sense signals from bacteria and their metabolites Han W. Tellez L.A. Perkins M.H. et al. A neural circuit for gut-induced reward. Cell. 2018; 175: 665-678.e23 Scopus (0) PubMed Abstract Full Text Full Text PDF Google Scholar and can be affected by the way bacteria interact with cells in the gut Bonaz B. Bazin T. Pellissier S. The vagus nerve at the interface of the microbiota-gut-brain axis. Front Neurosci. 2018; 12: 49 Scopus (229) PubMed Crossref Google Scholar For instance, bacteria produce fatty acids like butyrate, propionate, acetate, and valerate which can alter the way the gut works, such as how it moves, secretes, and reacts to inflammation. Bhattarai Y. Williams B.B. Battaglioli E.J. et al. Gut microbiota-produced tryptamine activates an epithelial G-protein-coupled receptor to increase colonic secretion. Cell Host Microbe. 2018; 23: 775-785.e5 Scopus (80) PubMed Abstract Full Text Full Text PDF Google ScholarStudies in mice suggest that the vagus nerve (which connects the brain to the gut) could be involved in how mood and behavior are linked to the gut microbiome.
For example, when mice had their vagus nerve cut, it blocked the brain's communication with certain bacteria in their gut, such as Lactobacillus and Bifidobacterium, which are important for controlling mood Bravo J.A. Forsythe P. Chew M.V. et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci U S A. 2011; 108: 16050-16055 Scopus (1661) PubMed Crossref Google Scholar Bercik P. Park A.J. Sinclair D. et al. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol Motil. 2011; 23: 1132-1139 Scopus (500) PubMed Crossref Google ScholarRecent research suggests that a two-way link exists between the gut microbiome, diet, and the vagus nerve, which could help explain how our mental health is linked to our gut.
When dietary tryptophan is increased, certain microbes make ECCs (Epithelial Cells of the Colon) more active Agus A. Planchais J. Sokol H. Gut microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe. 2018; 23: 716-724 Scopus (381) PubMed Abstract Full Text Full Text PDF Google Scholar ECCs also connect with nerves through special neuropod-like extensions Bohorquez D.V. Shahid R.A. Erdmann A. et al. Neuroepithelial circuit formed by innervation of sensory enteroendocrine cells. J Clin Invest. 2015; 125: 782-786 Scopus (182) PubMed Crossref Google Scholar The Autonomic Nervous System (ANS) can also make ECCs release serotonin into the gut, which gets taken up by special transporters and affects bacteria in the gut Sgritta M. Dooling S.W. Buffington S.A. et al. Mechanisms underlying microbial-mediated changes in social behavior in mouse models of autism spectrum disorder. Neuron. 2019; 101: 246-259.e6 PubMed Abstract Full Text Full Text PDF Google ScholarEnterochromaffin cells (ECCs) are a type of cell found in the digestive system that contains more than 90% of the body's serotonin (5-HT).
These cells can be activated by chemicals like short-chain fatty acids (SCFAs) and bile acids (2BAs) produced by certain bacteria in the gut. Eating more foods that contain the amino acid tryptophan can also increase the stimulatory effects of these ECCs, as it makes more of these chemicals available Yano J.M. Yu K. Donaldson G.P. et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015; 161: 264-276 Scopus (1106) PubMed Abstract Full Text Full Text PDF Google ScholarECCs also communicate with nerve endings in the gut by forming synaptic connections to them.
ECCs (enterochromaffin cells) can talk to different nerve cells by making connections with them.
The ANS (autonomic nervous system) can also make ECCs release 5-HT (a chemical) into the gut, which can be taken in by special molecules and impact the bacteria in the gut.
HIGHLIGHT
The Vagus Nerve's intricate connection to the gut, emotions, and microbiome, alongside ECCs' impact on gut-brain communication and bacteria.
The Crucial Role of Immunity in Gut-Brain Communication
Sensors and Signaling: Toll-like Receptors and Peptidoglycans in Immune Response
Immunity plays a vital role in connecting the gut microbiota, the ENS (Enteric Nervous System), and the brain. There are two types of sensors, Toll-like receptors (TLRs) and peptidoglycans (PGNs), which help the immune system to respond to microbes Rakoff-Nahoum S. Paglino J. Eslami-Varzaneh F. et al. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004; 118: 229-241 Scopus (2984) PubMed Abstract Full Text Full Text PDF Google Scholar Chu H. Mazmanian S.K. Innate immune recognition of the microbiota promotes host-microbial symbiosis. Nat Immunol. 2013; 14: 668-675 Scopus (290) PubMed Crossref Google Scholar . A healthy gut barrier stops the wrong activation of immune cells and the growth of systemic immune activation.Gut Bacteria's Impact on Brain Health: Immune Agonists, TLRs, and Neurological Diseases
Bacteria can release molecules called immune agonists such as lipopolysaccharide (LPS) and PGN, which can travel to the brain and interact with receptors called TLRs.
Scientists think that these TLRs play a role in diseases such as Alzheimer's Disease Lin C. Zhao S. Zhu Y. et al. Microbiota-gut-brain axis and toll-like receptors in Alzheimer's disease. Comput Struct Biotechnol J. 2019; 17: 1309-1317 Scopus (15) PubMed Crossref Google Scholar , Parkinson's Disease Perez-Pardo P. Dodiya H.B. Engen P.A. et al. Role of TLR4 in the gut-brain axis in Parkinson's disease: a translational study from men to mice. Gut. 2019; 68: 829-843 Scopus (38) PubMed Crossref Google Scholar , pain Tramullas M. Finger B.C. Moloney R.D. et al. Toll-like receptor 4 regulates chronic stress-induced visceral pain in mice. Biol Psychiatry. 2014; 76: 340-348 PubMed Abstract Full Text Full Text PDF Google Scholar , ,and depression Kelly J.R. Clarke G. Cryan J.F. et al. Brain-gut-microbiota axis: challenges for translation in psychiatry. Ann Epidemiol. 2016; 26: 366-372 Scopus (79) PubMed Crossref Google ScholarWhen mice are given antibiotics or special diets, the expression of certain receptors that detect PGN in the brain is reduced, suggesting that the bacteria in the gut can affect the brain.
Behavioral Consequences: Gut-Microbiota Interaction and Behavior Changes
It has been shown that altering the ability of mice to sense a particular type of bacteria (called peptidoglycan) can lead to changes in their behavior Arentsen T. Qian Y. Gkotzis S. et al. The bacterial peptidoglycan-sensing molecule Pglyrp2 modulates brain development and behavior. Mol Psychiatry. 2017; 22: 257-266 Scopus (96) PubMed Crossref Google ScholarThis suggests that the way that our bodies interact with bacteria can have important consequences for our behavior.
Diet can also affect the types of bacteria in our gut, which can lead to changes in the protective layer that stops bacteria from reaching cells in our body. This could result in our bodies reacting to both helpful and harmful bacteria.
Nutrition's Role in Immune Activation and Brain Health
The food we eat can cause our bodies to release chemicals that activate our immune systems Andre P. Laugerette F. Feart C. Metabolic endotoxemia: a potential underlying mechanism of the relationship between dietary fat intake and risk for cognitive impairments in humans?. Nutrients. 2019; 11: 1887-1910 Scopus (8) Crossref Google ScholarThis low level of immune system activation can affect different parts of our body, including our brain, and has been linked to depression and diseases like Alzheimer's and Parkinson's.
HIGHLIGHT
Immunity's role in connecting the gut, ENS, and brain, involves sensors like TLRs and PGNs.
The Impact of Antibiotics and Gut Bacteria on Neural and Immune Systems
TLR4 and TLR2: Key Players in Antibiotic-Induced Gut Changes
It has been suggested that the effects of germ-free and antibiotic-treated mice, such as decreased numbers of nitrergic neurons and reduced motility, may be caused by TLR4 and/or TLR2.
TLR2-deficient mice have also been shown to have issues in the way their neurons code the ENS, resulting in gut dysmotility and reduced chloride production in intestine explants Brun P. Giron M.C. Qesari M. et al. Toll-like receptor 2 regulates intestinal inflammation by controlling integrity of the enteric nervous system. Gastroenterology. 2013; 145: 1323-1333 Scopus (150) PubMed Abstract Full Text Full Text PDF Google ScholarAntibiotic use can change the amount of bacteria in the body, which can affect how our body responds to certain things.
This can lead to changes in the way our digestive system works, and how it reacts to a chemical called acetylcholine Grasa L. Abecia L. Forcen R. et al. Antibiotic-induced depletion of murine microbiota induces mild inflammation and changes in toll-like receptor patterns and intestinal motility. Microb Ecol. 2015; 70: 835-848 Scopus (10) PubMed Crossref Google ScholarIt looks like these changes might be caused, at least in part, by two things called TLR4 and TLR2.
Macrophages and Gut Bacteria: Collaborative Defense of the Digestive System
Macrophages are special cells that are found all over the gut Farache J. Zigmond E. Shakhar G. et al. Contributions of dendritic cells and macrophages to intestinal homeostasis and immune defense. Immunol Cell Biol. 2013; 91: 232-239 Scopus (89) PubMed Crossref Google Scholar . They help the body repair itself after injury. Studies have found that when people or animals are given antibiotics or don't have any bacteria living in their bodies (germ-free or GF mice), the number of macrophages found in the gut goes down Muller P.A. Koscso B. Rajani G.M. et al. Crosstalk between muscularis macrophages and enteric neurons regulates gastrointestinal motility. Cell. 2014; 158: 1210 Scopus (26) PubMed Abstract Full Text Full Text PDF Google ScholarThis suggests that the bacteria in our bodies have a role in helping to recruit and create macrophages.
Studies have shown that the bacteria in the gut can interact with the brain and the immune system to protect the digestive system.
For example, when a person is infected with Salmonella Typhimurium, the nerve cells in the digestive system can be activated by the bacteria and then the macrophages (a type of white blood cell) can be stimulated to help protect the nervous system and improve gut movement Gabanyi I.Muller P.A. Feighery L. et al. Neuro-immune interactions drive tissue programming in intestinal macrophages. Cell. 2016; 164: 378-391 Scopus (257) PubMed Abstract Full Text Full Text PDF Google Scholar The digestive system can also protect itself from Salmonella by producing a substance called IL-18, which helps to keep the mucous membrane barrier strong and makes it harder for bacteria to enter Jarret A. Jackson R. Duizer C. et al. Enteric nervous system-derived IL-18 orchestrates mucosal barrier immunity. Cell. 2020; 180: 813-814 Scopus (2) PubMed Abstract Full Text Full Text PDF Google Scholar Finally, research has shown that the bacteria in the gut can influence messages sent from the brain to other parts of the body, such as the nervous system Muller P.A. Schneeberger M. Matheis F. et al. Microbiota modulate sympathetic neurons via a gut-brain circuit. Nature. 2020; 583: 441-446 Scopus (33) PubMed Crossref Google ScholarHIGHLIGHT
Antibiotics and germ-free conditions alter gut function through TLR4 and TLR2, while gut bacteria influence macrophage presence and protect the digestive system against infections, impacting gut-brain communication.
The Impact of Gut Bacteria on Brain Function and Communication
Neurotransmitters and Gut Bacteria
The bacteria in our gut produce chemicals that can change the way our brains and nerves work.
These chemicals, called neurotransmitters, have been shown to exist in some bacteria in laboratory tests Taj A. Jamil N. Bioconversion of tyrosine and tryptophan derived biogenic amines by neuropathogenic bacteria. Biomolecules. 2018; 8: 10-19 Scopus (4) Crossref Google Scholar Roshchina V.V. New trends and perspectives in the evolution of neurotransmitters in microbial, plant, and animal cells. Adv Exp Med Biol. 2016; 874: 25-77 Scopus (46) PubMed Crossref Google ScholarBut it's not yet known if these neurotransmitters can get to the parts of the brain they need to, or if there are enough of them to make a difference.
Most neurotransmitters have a short lifespan and can't easily get through something called the blood-brain barrier, which makes it unlikely that they would be able to do much.
Serotonin and Tryptophan Metabolites
Research shows that serotonin and other tryptophan metabolites play a crucial role in gut-brain communication, affecting various aspects such as gastrointestinal motility, mood, and behavior Li Z. Chalazonitis A. Huang Y.Y. et al. Essential roles of enteric neuronal serotonin in gastrointestinal motility and the development/survival of enteric dopaminergic neurons. J Neurosci. 2011; 31: 8998-9009 Scopus (236) PubMed Crossref Google Scholar Mawe G.M. Hoffman J.M. Serotonin signalling in the gut--functions, dysfunctions and therapeutic targets. Nat Rev Gastroenterol Hepatol. 2013; 10: 473-486 Scopus (429) PubMed Crossref Google Scholar Brummelte S. Mc Glanaghy E. Bonnin A. et al. Developmental changes in serotonin signaling: implications for early brain function, behavior and adaptation. Neuroscience. 2017; 342: 212-231 Scopus (98) PubMed Crossref Google ScholarRecent research has highlighted the pivotal role of serotonin (5-HT) in communication between the gut and brain.
Certain bacteria can increase serotonin levels in the gut and bloodstream, potentially alleviating gut-related disorders Furusawa Y. Obata Y. Fukuda S. et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013; 504: 446-450 Scopus (2194) PubMed Crossref Google ScholarThis is because these bacteria produce a substance called SCFAs, which increases the production of 5-HT by turning on Tph1 in certain cells
Furthermore, the Turicibacter sanguinis bacterium, which can take up serotonin, is important for its colonization in the gut and its influence on the human body Fung T.C. Vuong H.E. Luna C.D.G. et al. Intestinal serotonin and fluoxetine exposure modulate bacterial colonization in the gut. Nat Microbiol. 2019; 4: 2064-2073 Scopus (52) PubMed Crossref Google ScholarShort-Chain Fatty Acids
Gut bacteria produce substances called SCFA metabolites that can affect different parts of the body, such as the gut, brain, and immune system.
These metabolites act through FFARs on cells like epithelial cells, EECs, ECCs, immune cells, and neurons to help regulate things like movement, secretion, and communication between the gut and brain.
For example, research has found that giving acetate, propionate, and butyrate can help restore the normal shape of microglia in the brain of germ-free mice and reduce the negative consequences of stress Erny D. Hrabe de Angelis A.L. Jaitin D. et al. Host microbiota constantly control maturation and function of microglia in the CNS. Nat Neurosci. 2015; 18: 965-977 Scopus (1092) PubMed Crossref Google Scholar van de Wouw M. Boehme M. Lyte J.M. et al. Short-chain fatty acids: Microbial metabolites that alleviate stress-induced brain-gut axis alterations. J Physiol. 2018; 596: 4923-4944 Scopus (151) PubMed Crossref Google Scholar SCFAs may also affect the production of chemicals in the brain that help control emotion and behavior, like noradrenaline and dopamine, by changing the activity of enzymes involved in their creation Nankova B.B. Agarwal R. MacFabe D.F. et al. Enteric bacterial metabolites propionic and butyric acid modulate gene expression, including CREB-dependent catecholaminergic neurotransmission, in PC12 cells--possible relevance to autism spectrum disorders. PLoS One. 2014; 9e103740 Scopus (0) PubMed Crossref Google ScholarFurther research is needed to find out how much of the short-lived substances called SCFAs can actually reach the brain since they only last from 25 minutes to three hours.
Studies that look at the influence of SCFAs on brain activity and behavior have usually used levels of SCFAs that are much higher than what is produced by microbes MacFabe D.F. Cain N.E. Boon F. et al. Effects of the enteric bacterial metabolic product propionic acid on object-directed behavior, social behavior, cognition, and neuroinflammation in adolescent rats: relevance to autism spectrum disorder. Behav Brain Res. 2011; 217: 47-54 Scopus (199) PubMed Crossref Google ScholarInfluence of Psychotropic Drugs on Gut Microbiota
Some psychotropic drugs, including SSRIs, can have an effect on the bacteria that live in the gut.
This effect, known as the intestinal microbiota, could explain why some of these drugs can have a back-and-forth influence on the body. Cussotto S. Clarke G. Dinan T.G. et al. Psychotropics and the microbiome: a chamber of secrets. Psychopharmacology (Berl). 2019; 236: 1411-1432 Scopus (7) PubMed Crossref Google ScholarResearch has also shown that the bacteria in our gut can help the adult nervous system develop and work properly.
This happens when the bacteria activate something called 5-HT4 receptors and this helps to make sure that the nervous system is working correctly.
Lastly, the bacteria in our gut can also affect how our brain works by changing the amount of a chemical called tryptophan, which is involved in the production of serotonin, a chemical that helps our brain stay balanced.
Tryptophan Metabolism Beyond Serotonin
Male GF mice have significantly more tryptophan in their bodies than normal mice [56], and this leads to higher levels of serotonin and its byproduct, 5-hydroxy-indole acetic acid [56], in their brains. Clarke G. Grenham S. Scully P. et al. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry. 2013; 18: 666-673 Scopus (841) PubMed Crossref Google ScholarIt is not yet known if this affects the social skills of these mice, and more research is needed to find out.
In a study with rodents, a reduction in Lactobacilli caused by chronic stress led to an increase in the conversion of tryptophan to kynurenine Marin I.A. Goertz J.E. Ren T.T. et al. Microbiota alteration is associated with the development of stress-induced despair behavior. Scientific Reports. 2017; 7: 43859 Scopus (0) PubMed Crossref Google Scholar This can have a negative effect on the brain, causing inflammation and damage Kennedy P.J. Cryan J.F. Dinan T.G. et al. Kynurenine pathway metabolism and the microbiota-gut-brain axis. Neuropharmacology. 2017; 112: 399-412 Scopus (202) PubMed Crossref Google ScholarIndole: Gut-Brain Communication Molecule
The production of indole, which is mainly found in the gut, is caused by an enzyme called tryptophan hydroxylase.
It has been discovered that indole is present in the blood, brain, and stomach.
Scientists have been exploring how indole, which is made from tryptophan in the gut, could affect the communication between the gut and the brain Osadchiy V. Labus J.S. Gupta A. et al. Correlation of tryptophan metabolites with connectivity of extended central reward network in healthy subjects. PLoS One. 2018; 13e0201772 Scopus (31) PubMed Crossref Google Scholar Indoles have lots of positive effects on how the intestines and body work together to stay healthy Galligan J.J. Beneficial actions of microbiota-derived tryptophan metabolites. Neurogastroenterol Motil. 2018; 30 Scopus (22) PubMed Crossref Google Scholar But some indoles can have bad effects on the connection between the gut and the brain, which has been seen to cause depression-like behavior in tests with animals Gheorghe C.E. Martin J.A. Manriquez F.V. et al. Focus on the essentials: tryptophan metabolism and the microbiome-gut-brain axis. Curr Opin Pharmacol. 2019; 48: 137-145 Scopus (19) PubMed Crossref Google ScholarTryptamine: Gut-Bacteria-Produced Molecule
Recent studies have shown that bacteria in our gut can produce a molecule called tryptamine that can affect the movement of food through our digestive system Bhattarai Y. Williams B.B. Battaglioli E.J. et al. Gut microbiota-produced tryptamine activates an epithelial G-protein-coupled receptor to increase colonic secretion. Cell Host Microbe. 2018; 23: 775-785.e5 Scopus (80) PubMed Abstract Full Text Full Text PDF Google ScholarThis suggests that bacteria in our gut are capable of producing molecules that affect how our bodies work.
It's not yet clear if these molecules can get into the brain and change our behavior Cohen L.J. Esterhazy D. Kim S.H. et al. Commensal bacteria make GPCR ligands that mimic human signalling molecules. Nature. 2017; 549: 48-53 Scopus (177) PubMed Crossref Google Scholar Colosimo D.A. Kohn J.A. Luo P.M. et al. Mapping interactions of microbial metabolites with human G-protein-coupled receptors. Cell Host Microbe. 2019; 26: 273-282.e7 Scopus (39) PubMed Abstract Full Text Full Text PDF Google ScholarHIGHLIGHT
Gut bacteria produce neurotransmitters and compounds like serotonin and SCFAs, influencing brain function and gut-brain communication, but their reach and effects on behavior remain uncertain.
Probiotics and Emotional Brain Power: Unveiling the Gut-Brain Connection

HIGHLIGHT
Probiotics can impact brain responses to emotions in both men and women, affecting stress levels and emotional decision-making, but their influence on behavior remains inconclusive in small-scale studies.
Disorders of Brain-Gut Interactions: IBS
The Intricate Relationship between IBS and Anxiety
IBS is a very common problem that affects up to 4.8% of people around the world Endo Y. Shoji T. Fukudo S. Epidemiology of irritable bowel syndrome. Ann Gastroenterol. 2015; 28: 158-159 PubMed Google ScholarIt happens when the brain and the digestive system don't work together well.
People with IBS feel pain in their stomachs and have changes to their digestion Drossman D.A. Hasler W.L. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016; 150: 1257-1261 PubMed Abstract Full Text Full Text PDF Google Scholar , even if there is nothing wrong with their body. It has been found that up to 50% of people who have an anxiety disorder also have IBS, and people with IBS are more than three times as likely to have an anxiety disorder Zamani M. Alizadeh-Tabari S. Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2019; 50: 132-143 Scopus (47) PubMed Crossref Google Scholar Sykes M.A. Blanchard E.B. Lackner J. et al. Psychopathology in irritable bowel syndrome: support for a psychophysiological model. J Behav Med. 2003; 26: 361-372 Scopus (121) PubMed Crossref Google Scholar Many IBS patients experienced difficult events or stressful situations in childhood or adulthood Halland M. Almazar A. Lee R. et al. A case-control study of childhood trauma in the development of irritable bowel syndrome. Neurogastroenterol Motil. 2014; 26: 990-998 Scopus (22) PubMed Crossref Google Scholar , but for some IBS starts after an event in the intestines. Sykes M.A. Blanchard E.B. Lackner J. et al. Psychopathology in irritable bowel syndrome: support for a psychophysiological model. J Behav Med. 2003; 26: 361-372 Scopus (121) PubMed Crossref Google ScholarA study was done to look at people with anxiety/depression and IBS and people with neither condition, and it showed how the brain and gut work together.
It has been concluded from the study that people who have higher levels of anxiety and depression at the start are more likely to develop IBS.
On the other hand, those who have IBS at the beginning show higher levels of anxiety or depression.
Surprisingly, in two out of three situations, the diagnosis of IBS came first, suggesting that in some people, having a problem with their stomach can be the cause of a mood disorder Koloski N.A. Jones M. Talley N.J. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016; 44: 592-600 Scopus (98) PubMed Crossref Google ScholarThe Brain's Role in Stomach Pain: Insights from fMRI Scans
Changes in the way the brain works, as seen on an fMRI scan, may be related to stomach pain Mayer E.A. Labus J. Aziz Q. et al. Role of brain imaging in disorders of brain-gut interaction: a Rome Working Team Report. Gut. 2019; 68: 1701-1715 Scopus (25) PubMed Crossref Google ScholarScientists have discovered that parts of the brain that help control anxiety and how the body deals with things, like the amygdala, are linked to how sensitive the colon is and how well the intestines move.
Research has found links between brain networks that can cause anxiety, like the amygdala, and parts of the body that are related to digestion, such as the colon and intestines.
Scientists have also noticed changes in pain signals in the brain when it comes to feeling emotions and dealing with digestive issues . Wilder-Smith C.H. Schindler D. Lovblad K. et al. Brain functional magnetic resonance imaging of rectal pain and activation of endogenous inhibitory mechanisms in irritable bowel syndrome patient subgroups and healthy controls. Gut. 2004; 53: 1595-1601 Scopus (305) PubMed Crossref Google Scholar Tillisch K. Mayer E.A. Labus J.S. Quantitative meta-analysis identifies brain regions activated during rectal distension in irritable bowel syndrome. Gastroenterology. 2011; 140: 91-100 Scopus (270) PubMed Abstract Full Text Full Text PDF Google Scholar This suggests that a similar process in rodents, which involves a stress hormone called corticotropin-releasing factor, may be involved in how the brain and gut are connected Tache Y. Bonaz B. Corticotropin-releasing factor receptors and stress-related alterations of gut motor function. J Clin Invest. 2007; 117: 33-40 Scopus (266) PubMed Crossref Google ScholarIBS and the Enigmatic Microbiome Connection
It is yet to be found out if the changes in the gut microbiota are responsible for IBS symptoms Simren M. Barbara G. Flint H.J. et al. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013; 62: 159-176 Scopus (548) PubMed Crossref Google Scholar Recent findings suggest that some IBS patients have similar gut microbial communities to healthy individuals, despite experiencing gastrointestinal symptoms, despite previous studies reporting different fecal microbial compositions in IBS patients based on factors such as age, type of IBS, and compartment. Labus J.S. Hollister E.B. Jacobs J. et al. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome. 2017; 5: 49 PubMed Crossref Google ScholarMoreover, one research study showed that a dysbiotic IBS subgroup had different brain volumes than a group with regular gut microbiota, which could demonstrate a connection between the microbial community structure and the brain structure.
Although people with IBS and healthy controls had the same type of microbiota, meaning that the bacteria in their gut were the same, it is unclear if dysbiosis (unbalance of bacteria in the gut) is the cause of IBS symptoms.
Studies have been done that found that the severity of IBS symptoms does appear to be related to dysbiosis Tap J. Derrien M. Tornblom H. et al. Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology. 2017; 152: 111-123e8 Scopus (216) PubMed Abstract Full Text Full Text PDF Google ScholarMore recently, research was done that showed that people with different types of IBS had different types of bacteria in their gut.
A recent study showed that people with different types of IBS had different amounts of "Clostridiales" in their digestive systems.
This was linked to different levels of "fecal SCFAs" and "fecal cytokine levels" Gargari G. Taverniti V. Gardana C. et al. Fecal Clostridiales distribution and short-chain fatty acids reflect bowel habits in irritable bowel syndrome. Environ Microbiol. 2018; 20: 3201-3213 Scopus (18) PubMed Crossref Google ScholarTo understand how these things are connected, more research is needed that looks at people without IBS and with a bigger sample size.
The Multifaceted Factors Influencing the IBS Microbiota
The findings from studies on the IBS microbiota can be attributed to the various technologies used to study the microbiota, the source of the sample, the different types of IBS, the effect of the autonomic nervous system on other aspects of the body (e.g. mucus production, intestinal permeability and mucosal immunity) . Osadchiy V. Martin C.R. Mayer E.A. The gut-brain axis and the microbiome: mechanisms and clinical implications. Clin Gastroenterol Hepatol. 2019; 17: 322-332 Scopus (55) PubMed Abstract Full Text Full Text PDF Google Scholar As well as other factors that can influence microbial composition and function (e.g. age, diet, antibiotic exposure, geography, probiotic intake, medication use) Kang D.W. Park J.G. Ilhan Z.E. et al. Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PLoS One. 2013; 8e68322 Scopus (463) PubMed Crossref Google ScholarThis is further complicated by the need to take into account the effect of the brain and nervous system on gut physiology and motility, such as sleep quality and stress.
Unveiling the Serotonin Puzzle: A Key to Understanding IBS
It appears that alterations in enteric mucosal and blood serotonin signaling have been observed in both adults and children who have Irritable Bowel Syndrome (IBS).
This could be an indicator of a disruption in the communication between the gut and the brain. Serotonin is a chemical that can activate more than 15 different receptors and subtypes in the brain and in the intestine.
A lot of the research into IBS has focused on two of these receptors called the 5-HT3 and 5-HT4 receptors, as they have been linked to mood, motility, and abdominal pain. Rebholz H. Friedman E. Castello J. Alterations of expression of the serotonin 5-HT4 receptor in brain disorders. Int J Mol Sci. 2018; 19: 3581-3601 Scopus (19) Crossref Google Scholar Gershon M.D. 5-Hydroxytryptamine (serotonin) in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes. 2013; 20: 14-21 Scopus (292) PubMed Crossref Google ScholarHIGHLIGHT
IBS is a common condition affecting digestion and is often linked to anxiety. The gut microbiome's role is unclear, but stress and serotonin signaling disruptions are associated with IBS. Brain-gut interactions play a key role in the condition's complexity.
Gut Bacteria: The Hidden Link to Mental Health
In recent years, there have been a lot of studies showing that people with Major Depressive Disorder (MDD) have a different makeup of bacteria in their gut compared to people who are healthy Valles-Colomer M. Falony G. Darzi Y. et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol. 2019; 4: 623-632 Scopus (386) PubMed Crossref Google Scholar
This difference in results is likely because of the same things that cause Irritable Bowel Syndrome.
The findings of studies suggest that the same reasons that cause irritable bowel syndrome (IBS) may also be responsible for different outcomes in mental health.
It has been observed that when the microbiome of a depressed person is transferred to a healthy mouse, it can produce symptoms of depression in the mouse, suggesting that the microbiome may play an important role in the development of depression.
This opens up the concept that targeting the microbiome might help improve mental health Zheng P. Zeng B. Zhou C. et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host's metabolism. Mol Psychiatry. 2016; 21: 786-796 PubMed Crossref Google ScholarHIGHLIGHT
Recent research links Major Depressive Disorder to distinct gut bacteria, akin to Irritable Bowel Syndrome, suggesting the gut microbiome's potential influence on mental health.
Mood and IBS: Targeting the MGB Axis
Dietary Interventions for IBS and Mental Well-being
Research has found that when adults with IBS-D follow a low FODMAP diet, their symptoms, quality of life, anxiety, and activity levels improve Algera J. Colomier E. Simren M. The dietary management of patients with irritable bowel syndrome: a narrative review of the existing and emerging evidence. Nutrients. 2019; 11: 2162-2184 Scopus (9) Crossref Google ScholarHowever, this diet may not be suitable for long-term use, as it could reduce the diversity and abundance of the gut microbiome, as well as be difficult to maintain for a long period of time.
Nutritional Psychiatry is a different way of treating depression. Studies have shown that eating a mostly plant-based diet, such as the traditional Mediterranean diet, can help with depression Dinan T.G. Stanton C. Long-Smith C. et al. Feeding melancholic microbes: MyNewGut recommendations on diet and mood. Clin Nutr. 2019; 38: 1995-2001 Scopus (0) PubMed Abstract Full Text Full Text PDF Google ScholarScientists do not yet know exactly how food affects our moods or which ingredients are the most helpful, but they are working on finding out.
Supplementing the Gut Microbiome: The Probiotic Dilemma
Probiotics have been tried as an alternate treatment to help with mental health, but so far, there is no proof that they actually work Huang R. Wang K. Hu J. Effect of probiotics on depression: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2016; 8: 483-495 Scopus (109) PubMed Crossref Google Scholar Research has shown that taking probiotics, such as types of Bifidobacterium and Lactobacillus, or VSL#3, can help reduce the symptoms of IBS for both adults and children Horvath A. Dziechciarz P. Szajewska H. Meta-analysis: Lactobacillus rhamnosus GG for abdominal pain-related functional gastrointestinal disorders in childhood. Aliment Pharmacol Ther. 2011; 33: 1302-1310 Scopus (130) PubMed Crossref Google Scholar Preidis G.A. Weizman A.V. Kashyap P.C. et al. AGA technical review on the role of probiotics in the management of gastrointestinal disorders. Gastroenterology. 2020; 159: 708-738 Scopus (18) PubMed Abstract Full Text Full Text PDF Google Scholar Su G.L. Ko C.W. Bercik P. et al. AGA Clinical Practice Guidelines on the Role of Probiotics in the Management of Gastrointestinal Disorders. Gastroenterology. 2020; 159: 697-705 Scopus (34) PubMed Abstract Full Text Full Text PDF Google ScholarThe recently published AGA Guidelines on probiotics do not recommend their use in IBS, due to the fact that the quality of the studies is not good enough, other than in controlled studies.
Probiotic supplements can alter the gut microbiota in humans, but the extent of the changes varies.
Advanced technologies like metagenomics or metabolomics should be utilized to accurately evaluate the impact of probiotic interventions on gut microbial profiles.
Fecal Microbiome Transplantation (FMT) in IBS and Mood Disorders
Research into fecal microbiota transplantation (FMT) is still limited, and no clear benefit has been found when looking at the results of studies as a whole Xu D. Chen V.L. Steiner C.A. et al. Efficacy of fecal microbiota transplantation in irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2019; 114: 1043-1050 Scopus (0) PubMed Crossref Google ScholarTwo recent studies that compared FMT to other treatments found changes in the gut microbiome of those who had the FMT.
Two recent studies have shown changes in the bacteria in the guts of people who received an FMT (a type of medical treatment).
In one study, those receiving the FMT reported a significant reduction in IBS symptoms three months later.
However, in the other study, those who received a placebo (a type of dummy treatment) reported greater improvement in their symptoms. Scientists are currently working on more detailed studies to see if FMT could help with depression. El-Salhy M. Hatlebakk J.G. Gilja O.H. et al. Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut. 2020; 69: 859-867 Scopus (64) PubMed Crossref Google ScholarHIGHLIGHT
A low FODMAP diet aids IBS-D symptoms but isn't long-term friendly. Plant-based diets show promise for depression. Probiotics' mental health effects remain inconclusive. FMT research yields mixed results; potential for IBS, exploring depression.
Shaping the Future of Medicine: Microbiome Insights into Brain Disorders

Significant advancements have been made in comprehending the MGB axis in preclinical models of human brain disorders, and in exploring the potential translation of these discoveries into clinical applications.
Research has established that brain-gut interaction disorders such as IBS have a strong neurological component and that numerous brain disorders have gastrointestinal implications, or may even originate from the gut.
Although the causal relationship between the gut microbiome and these interactions is yet to be established, this valuable knowledge will undoubtedly shape the development of interdisciplinary therapeutic approaches for years to come.
The microbiome (the collection of bacteria living in our bodies) can have a different effect on brain development in males and females.
Girls are more likely to suffer from stress-related and functional GI disorders Audet M.C. Stress-induced disturbances along the gut microbiota-immune-brain axis and implications for mental health: does sex matter?. Front Neuroendocrinol. 2019; 54: 100772 Scopus (23) PubMed Crossref Google Scholar Vemuri R. Sylvia K.E. Klein S.L. et al. The microgenderome revealed: sex differences in bidirectional interactions between the microbiota, hormones, immunity and disease susceptibility. Semin Immunopathol. 2019; 41: 265-275 Scopus (55) PubMed Crossref Google Scholar , while animal studies suggest that boys are more vulnerable to problems with the microbiome early on in life Jaggar M. Rea K. Spichak S. et al. You've got male: sex and the microbiota-gut-brain axis across the lifespan. Front Neuroendocrinol. 2020; 56: 100815 Scopus (31) PubMed Crossref Google ScholarRecent studies have found that male brains seem to be more sensitive to changes in the bacteria living in their gut compared to female brains.
This has led to scientists wanting to learn more about how these changes affect different genders Mulak A. Tache Y. Larauche M. Sex hormones in the modulation of irritable bowel syndrome. World J Gastroenterol. 2014; 20: 2433-2448 Scopus (104) PubMed Crossref Google Scholar However, there has been no research into how race might impact the bacteria in our gut and its effects on the brain Royston K.J. Adedokun B. Olopade O.I. Race, the microbiome and colorectal cancer. World J Gastrointest Oncol. 2019; 11: 773-787 Scopus (0) PubMed Crossref Google ScholarInvestigations are currently being done to develop live biotherapeutics, which are bacteria-made substances that have positive impacts on the brain. This field is still in its early stages.
To treat conditions such as irritable bowel syndrome (IBS) and other disorders that involve interactions between the gut and the brain, the best treatments involve a combination of personalized diet plans, behavioral therapies, and a few medications that can help improve digestive function Simren M. Tack J. New treatments and therapeutic targets for IBS and other functional bowel disorders. Nat Rev Gastroenterol Hepatol. 2018; 15: 589-605 Scopus (45) PubMed Crossref Google ScholarThere are pathways connecting the gut and the brain, and understanding them can help us treat these conditions better.
HIGHLIGHT
Recent research reveals a strong link between the gut and brain, especially in disorders like IBS. Gender differences in microbiome impact are being explored, while live biotherapeutics show promise. Understanding gut-brain connections informs effective treatments.
Discussion
The information provided underscores the intricate relationship between the gut, brain, and overall health.
The gut-brain connection is mediated by neurotransmitters like serotonin, which are influenced by specific bacteria in the gut.
This connection has implications for various conditions, including IBS and mood disorders.
Psychotropic medications, like SSRIs, may not only affect brain function but also have a bidirectional impact on gut bacteria.
The gut microbiota plays a role in the development and functioning of the nervous system through 5-HT4 receptors, shedding light on the importance of gut health for overall well-being.
The gut microbiota's potential role in mental health is a topic of significant interest. Studies suggest that differences in gut bacteria composition may contribute to conditions like Major Depressive Disorder.
Probiotics and dietary changes have shown some promise in managing both gut and mood disorders, but further research is necessary to confirm their effectiveness.
Fecal microbiota transplantation (FMT) is being explored as a potential treatment for altering gut bacteria and improving symptoms in conditions like IBS. However, its efficacy is still a subject of ongoing research.
The Microbiome-Gut-Brain (MGB) axis is a complex system that connects gut health with brain function. Understanding this axis can lead to innovative interdisciplinary therapies.
Conclusion
The gut-brain connection, mediated by neurotransmitters like serotonin and influenced by specific gut bacteria, is a critical aspect of overall health.
It has implications for conditions like IBS and mood disorders, highlighting the importance of maintaining a healthy gut microbiota.
Further research is needed to better understand the exact mechanisms and to develop effective treatments that harness the potential of the gut-brain axis for improved well-being.
Review date not set.
How we reviewed this article:
Latest on:





