5 Secrets of the Gut-Spine Axis Revealed
Discover the top 5 secrets of the Gut-Spine Axis and learn how gut microbiota plays a crucial role in maintaining a healthy spine.

In This Article:
Key Points
- Gut-Spine Axis: The Gut Microbiota (GM) is pivotal for spine health, influencing metabolism, immunity, and the gut-brain-bone connection. Dysbiosis in GM can lead to Spinal Degenerative Diseases (SDD) through impaired nutrient absorption, immune disruptions, and altered neurotransmitter levels.
- Gut Microbiota and Bone Health: GM has a profound impact on bone health, with osteoporosis and hyperostotic diseases being influenced by immune-inflammatory mechanisms. Research indicates a strong connection between GM composition and osteoporosis, suggesting the "gut-bone axis" as a potential therapeutic target.
- Gut-Joint Linkage: The emerging "gut-joint axis" concept delves into the relationship between gut and joint health. GM dysbiosis is associated with Osteoarthritis (OA), suggesting that bacterial imbalances might accelerate OA conditions.
- Gut-Disk and Gut-Ligament Interactions: The "gut-disk axis" emphasizes the relationship between GM dysbiosis and Intervertebral Disc Degeneration (IVDD), with microbial differences noted between healthy and degenerated discs. Additionally, while a direct "gut-ligament axis" hasn't been established, it presents an intriguing area for exploration in Lumbar Spinal Stenosis.
- Gut Influence on Muscles and Pain: Spinal sarcopenia's connection with GM highlights the "gut-muscle axis", emphasizing the role of microbiota in muscle health. Additionally, GM plays a central role in pain modulation associated with Spinal Degenerative Diseases, producing pain-regulating compounds and neurotransmitters, which suggests the need for careful selection of analgesics in SDD pain treatment.
Secrets of the Gut-Spine Axis: A Modern Perspective
The Gut Microbiota (GM) plays an integral role in maintaining the balance and health of our spine and its various components, including bones, cartilage, disks, ligaments, and muscles A Trusted Source Behera, J., Ison, J., Tyagi, S. C., and Tyagi, N. (2020). The role of gut microbiota in bone homeostasis.Bone135:115317. doi: 10.1016/j.bone.2020.115317 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Seely, K. D., Kotelko, C. A., Douglas, H., Bealer, B., and Brooks, A. E. (2021). The human gut microbiota: a key mediator of osteoporosis and osteogenesis.Int. J. Mol. Sci.22:9452. doi: 10.3390/ijms22179452 PubMed AbstractCrossRef Full TextGoogle Scholar .
GM affects our metabolism, immunity, endocrine environment, and even the gut-brain-bone connection.
When there's an imbalance in the GM, known as dysbiosis, the health of our spinal structures can be compromised through several mechanisms.

This includes impaired nutrient absorption (e.g., calcium, amino acids, and vitamin K), disrupted immune regulation involving estrogen and short-chain fatty acids (SCFA),
and altered neurotransmitter levels, such as serotonin and leptin, which are crucial for bone metabolism A Trusted Source Chen, Y., Wang, X., Zhang, C., Liu, Z., Li, C., and Ren, Z. (2022b). Gut microbiota and bone diseases: a growing partnership.Front. Microbiol.13:877776. doi: 10.3389/fmicb.2022.877776 PubMed AbstractCrossRef Full TextGoogle Scholar .
This imbalance can lead to various Spinal Degenerative Diseases (SDD), such as osteoporosis, osteoarthritis (OA), and Intervertebral Disc Degeneration (IVDD),
further exacerbated by the accumulation of senescent cells and systemic inflammation A Trusted Source Borghesan, M., Hoogaars, W. M. H., Varela-Eirin, M., Talma, N., and Demaria, M. (2020). A senescence-centric view of aging: implications for longevity and disease.Trends Cell Biol.30, 777–791. doi: 10.1016/j.tcb.2020.07.002 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Sharma, R. (2022). Emerging interrelationship between the gut microbiome and cellular senescence in the context of aging and disease: perspectives and therapeutic opportunities.Probiotics Antimicrob. Proteins14, 648–663. doi: 10.1007/s12602-021-09903-3 PubMed AbstractCrossRef Full TextGoogle Scholar .
Role of Gut Microbiota in Bone Health and Disease
The Spinal Degenerative Diseases (SDD) associated with bone metabolism include osteoporotic vertebral fractures (OVF) and hyperostotic diseases such as ossification of the posterior longitudinal ligament (OPLL)
and diffuse idiopathic skeletal hyperostosis (DISH) A Trusted Source Zaiss, M. M., Jones, R. M., Schett, G., and Pacifici, R. (2019). The gut-bone axis: how bacterial metabolites bridge the distance.J. Clin. Invest.129, 3018–3028. doi: 10.1172/JCI128521PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Mader, R., Pappone, N., Baraliakos, X., Eshed, I., Sarzi-Puttini, P., Atzeni, F., et al. (2021). Diffuse idiopathic skeletal hyperostosis (DISH) and a possible inflammatory component.Curr. Rheumatol. Rep.23:6. doi: 10.1007/s11926-020-00972-xCrossRef Full TextGoogle Scholar A Trusted Source Kawaguchi, Y. (2022). Biomarker research approach to the pathogenesis of ossification of the spinal ligament: a review.Spine Surg. Relat. Res.6, 224–232. doi: 10.22603/ssrr.2021-0229 PubMed AbstractCrossRef Full TextGoogle Scholar .
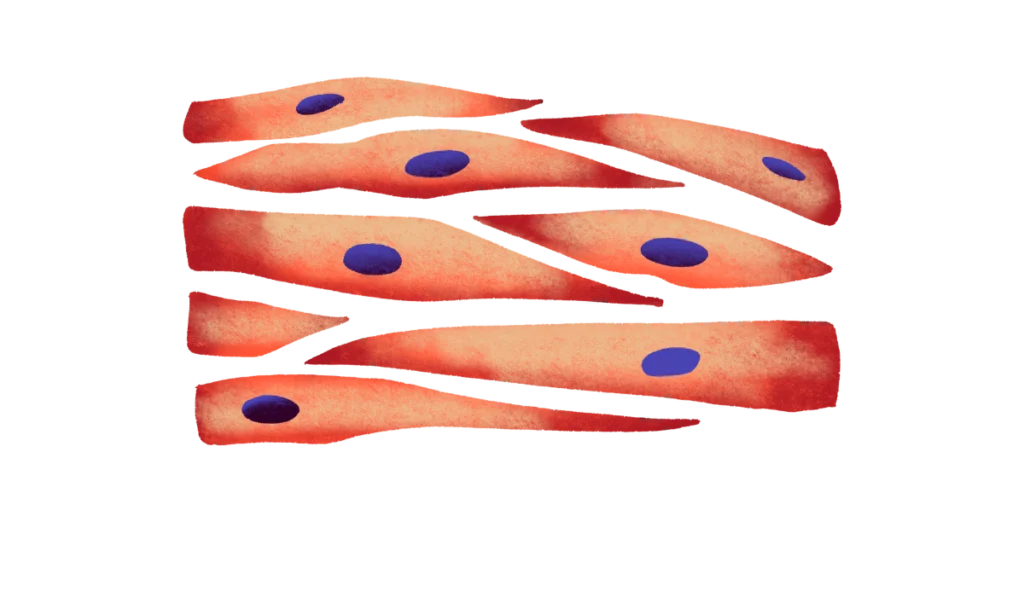
Osteoporosis and hyperostotic diseases share an immune-inflammatory mechanism in their pathogenesis, with bone health hinging on the balance between osteoblasts and osteoclasts.
Inflammatory diseases engage various cytokines that influence the osteoblast-osteoclast equilibrium, making immune activity a crucial factor in osteoporosis A Trusted Source Arron, J. R., and Choi, Y. (2000). Bone versus immune system.Nature408, 535–536. doi: 10.1038/35046196 PubMed AbstractCrossRef Full TextGoogle Scholar.
The term "osteoimmunology" aptly describes the symbiotic relationship between the immune system and bone metabolism, highlighting the role of immune cells or factors in skeletal development A Trusted Source Takayanagi, H. (2021). Osteoimmunology as an intrinsic part of immunology.Int. Immunol.33, 673–678. doi: 10.1093/intimm/dxab057 PubMed AbstractCrossRef Full TextGoogle Scholar .
Research has established the impact of Gut Microbiota (GM) on bone tissue, evidenced by studies on GM-free mice, animals fed GM-modifying antibiotics and diets, and humans A Trusted Source Ibáñez, L., Rouleau, M., Wakkach, A., and Blin-Wakkach, C. (2019). Gut microbiome and bone.Joint Bone Spine86, 43–47. doi: 10.1016/j.jbspin.2018.02.008 PubMed AbstractCrossRef Full TextGoogle Scholar .
Notably, osteoporosis correlates with GM composition and diversity A Trusted Source Wang, J., Wang, Y., Gao, W., Wang, B., Zhao, H., Zeng, Y., et al. (2017). Diversity analysis of gut microbiota in osteoporosis and osteopenia patients.PeerJ5:e3450. doi: 10.7717/peerj.3450 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Ling, C. W., Miao, Z., Xiao, M. L., Zhou, H., Jiang, Z., Fu, Y., et al. (2021). The association of gut microbiota with osteoporosis is mediated by amino acid metabolism: multiomics in a large cohort.J. Clin. Endocrinol. Metab.106, e3852–e3864. doi: 10.1210/clinem/dgab492 PubMed AbstractCrossRef Full TextGoogle Scholar .
In the realm of osteoimmunology, GM dysbiosis has been reported to contribute to osteoporosis and potentially influence hyperostosis diseases.
Obesity, type 2 diabetes mellitus, and metabolic syndrome complications, all characterized by low-grade systemic inflammation,
are strongly associated with hyperostotic diseases like OPLL and DISH A Trusted Source Mader, R., Pappone, N., Baraliakos, X., Eshed, I., Sarzi-Puttini, P., Atzeni, F., et al. (2021). Diffuse idiopathic skeletal hyperostosis (DISH) and a possible inflammatory component.Curr. Rheumatol. Rep.23:6. doi: 10.1007/s11926-020-00972-x CrossRef Full TextGoogle Scholar A Trusted Source Kawaguchi, Y. (2022). Biomarker research approach to the pathogenesis of ossification of the spinal ligament: a review.Spine Surg. Relat. Res.6, 224–232. doi: 10.22603/ssrr.2021-0229 PubMed AbstractCrossRef Full TextGoogle Scholar .

Moreover, OPLL is linked to leptin and chronic inflammation.
The Fascinating Connection Between Our Gut and Joint Health
Facet Joint Syndrome, a type of Spinal Degenerative Disease (SDD), results from the degeneration of cartilage in facet joints, leading to Osteoarthritis (OA) A Trusted Source Du, R., Xu, G., Bai, X., and Li, Z. (2022). Facet joint syndrome: pathophysiology, diagnosis, and treatment.J. Pain Res.15, 3689–3710. doi: 10.2147/JPR.S389602 CrossRef Full TextGoogle Scholar .
The "gut-joint axis" has emerged as a critical concept, exploring the potential cross-talk between our gut and joints, influencing conditions such as OA A Trusted Source Berthelot, J. M., Sellam, J., Maugars, Y., and Berenbaum, F. (2019). Cartilage-gut-microbiome axis: a new paradigm for novel therapeutic opportunities in osteoarthritis.RMD Open5:e001037. doi: 10.1136/rmdopen-2019-001037 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source De Sire, A., De Sire, R., Petito, V., Masi, L., Cisari, C., Gasbarrini, A., et al. (2020). Gut-joint axis: the role of physical exercise on gut microbiota modulation in older people with osteoarthritis.Nutrients12:574. doi: 10.3390/nu12020574 PubMed AbstractCrossRef Full TextGoogle Scholar .
While there hasn't been a direct association between Facet Joint Syndrome and Gut Microbiota (GM) yet, parallels can be drawn from the correlation between GM and lower-extremity OA.
Notably, obesity and metabolic syndrome, often associated with systemic chronic low-level inflammation, have been identified as risk factors for OA in both load-bearing and non-load-bearing joints A Trusted Source Yoshimura, N., Muraki, S., Oka, H., Tanaka, S., Kawaguchi, H., Nakamura, K., et al. (2012). Accumulation of metabolic risk factors such as overweight, hypertension, dyslipidaemia, and impaired glucose tolerance raises the risk of occurrence and progression of knee osteoarthritis: a 3-year follow-up of the ROAD study.Osteoarthr. Cartil.20, 1217–1226. doi: 10.1016/j.joca.2012.06.006 PubMed AbstractCrossRef Full TextGoogle Scholar .
Moreover, low levels of inflammation, often related to obesity/metabolic syndrome, aging, diet, and postmenopausal estrogen deficiency, play a significant role in the development and progression of OA A Trusted Source Li, Y., Luo, W., Deng, Z., and Lei, G. (2016). Diet-intestinal microbiota axis in osteoarthritis: a possible role.Mediat. Inflamm.2016:3495173. doi: 10.1155/2016/3495173 PubMed AbstractCrossRef Full TextGoogle Scholar .
GM dysbiosis has been linked to OA, with significant shifts in pathogenic microorganisms observed in OA patients A Trusted Source Favazzo, L. J., Hendesi, H., Villani, D. A., Soniwala, S., Dar, Q. A., Schott, E. M., et al. (2020). The gut microbiome-joint connection: implications in osteoarthritis.Curr. Opin. Rheumatol.32, 92–101. doi: 10.1097/BOR.0000000000000681 PubMed AbstractCrossRef Full TextGoogle Scholar .
Moreover, occult or subclinical bacterial infections from GM dysbiosis might accelerate OA, as microbes have been found in knee and hip OA A Trusted Source Dunn, C. M., Velasco, C., Rivas, A., Andrews, M., Garman, C., Jacob, P. B., et al. (2020). Identification of cartilage microbial DNA signatures and associations with knee and hip osteoarthritis.Arthritis Rheumatol.72, 1111–1122. doi: 10.1002/art.41210 PubMed AbstractCrossRef Full TextGoogle Scholar .
These findings support the potential application of the "gut-joint axis" concept to Facet OA and underscore the need for further research to establish this relationship in both basic and clinical settings.
Gut-Disk Connection
Intervertebral Disc Degeneration (IVDD) involves a complex interplay between the central gelatinous nucleus pulposus, outer annulus fibrosus, and cartilaginous endplates A Trusted Source Li, W., Lai, K., Chopra, N., Zheng, Z., Das, A., and Diwan, A. D. (2022). Gut-disc axis: a cause of intervertebral disc degeneration and low back pain.Eur. Spine J.31, 917–925. doi: 10.1007/s00586-022-07152-8 PubMed AbstractCrossRef Full TextGoogle Scholar .
IVDD's multifaceted nature often includes chronic low-grade inflammation as a key player in its development.
The unique structure of the Intervertebral Disc (IVD) creates a protective barrier, akin to the blood-brain barrier, shielding it from systemic infections.
However, damaged IVDs may become breeding grounds for anaerobic bacteria, which can bypass the body's immune responses A Trusted Source Wedderkopp, N., Thomsen, K., Manniche, C., Kolmos, H. J., Secher Jensen, T., and Leboeuf Yde, C. (2009). No evidence for presence of bacteria in modic type I changes.Acta Radiol.50, 65–70. doi: 10.1080/02841850802524485PubMed AbstractCrossRef Full TextGoogle Scholar .
These bacteria release inflammatory factors, such as IL-6 and TNFα, further recruiting inflammatory cells like T cells and macrophages, ultimately exacerbating IVDD A Trusted Source Schirmer, M., Smeekens, S. P., Vlamakis, H., Jaeger, M., Oosting, M., Franzosa, E. A., et al. (2016). Linking the human gut microbiome to inflammatory cytokine production capacity.Cells167, 1125–1136.e8. doi: 10.1016/j.cell.2016.10.020 PubMed AbstractCrossRef Full TextGoogle Scholar .
A fascinating twist in IVDD's tale involves Gut Microbiota (GM) dysbiosis, where an imbalance in the gut microbial ecosystem may lead to the migration of harmful microbes and their metabolites into the bloodstream and IVD, potentially worsening IVDD.
Research has even shown that the microbiome composition differs significantly between healthy and degenerated IVDs, introducing the "gut-disk axis" as a crucial element in understanding and potentially treating IVDD and associated low back pain A Trusted Source Rajasekaran, S., Soundararajan, D. C. R., Tangavel, C., Muthurajan, R., Sri Vijay Anand, K. S., Matchado, M. S., et al. (2020). Human intervertebral discs harbour a unique microbiome and dysbiosis determines health and disease.Eur. Spine J.29, 1621–1640. doi: 10.1007/s00586-020-06446-z PubMed AbstractCrossRef Full TextGoogle Scholar .
Gut-Ligament Connection in Lumbar Spinal Stenosis
Lumbar Spinal Stenosis (LSS) can often stem from the thickening of the yellow lumbar ligament, a process potentially fueled by inflammation-related scars A Trusted Source Sairyo, K., Biyani, A., Goel, V. K., Leaman, D. W., Booth, R., Thomas, J., et al. (2007). Lumbar ligamentum flavum hypertrophy is due to accumulation of inflammation-related scar tissue.Spine (Phila Pa 1976)32, E340–E347. doi: 10.1097/01.brs.0000263407.25009.6e PubMed AbstractCrossRef Full TextGoogle Scholar .
While LSS has been linked to diabetes, hypertension, and metabolic syndrome, all known associates of Gut Microbiota (GM) dysbiosis A Trusted Source Fujita, N. (2021). Lumbar spinal canal stenosis from the perspective of locomotive syndrome and metabolic syndrome: a narrative review.Spine Surg. Relat. Res.5, 61–67. doi: 10.22603/ssrr.2020-0112 PubMed AbstractCrossRef Full TextGoogle Scholar , a direct link between LSS and GM remains unreported.
However, considering that both Intervertebral Disc Degeneration (IVDD) and facet Osteoarthritis (OA), known factors of LSS, have relationships with GM, the likelihood of a "gut-ligament axis" influencing LSS is a tantalizing possibility that warrants further exploration.
Gut-Muscle Link in Spinal Sarcopenia
Spinal sarcopenia, a decline in muscle mass, strength, and function, is intricately connected to the composition and diversity of our gut microbiota (GM) A Trusted Source Cruz-Jentoft, A. J., Bahat, G., Bauer, J., Boirie, Y., Bruyère, O., Cederholm, T., et al. (2019). Sarcopenia: revised European consensus on definition and diagnosis.Age Ageing48, 16–31. doi: 10.1093/ageing/afy169 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Picca, A., Fanelli, F., Calvani, R., Mulè, G., Pesce, V., Sisto, A., et al. (2018). Gut dysbiosis and muscle aging: searching for novel targets against sarcopenia.Mediat. Inflamm.2018:7026198. doi: 10.1155/2018/7026198 PubMed AbstractCrossRef Full TextGoogle Scholar .
Disruptions in GM can lead to inflammation, immunity challenges, and mitochondrial dysfunction, all of which can contribute to sarcopenia in the spine, ultimately impacting our overall well-being.
Research has shown significant differences in GM between individuals with and without sarcopenia, indicating a crucial "gut-muscle axis" that facilitates communication between the gut and skeletal muscles A Trusted Source Kuo, Y. K., Lin, Y. C., Lee, C. Y., Chen, C. Y., Tani, J., Huang, T. J., et al. (2020). Novel insights into the pathogenesis of spinal sarcopenia and related therapeutic approaches: a narrative review.Int. J. Mol. Sci.21:3010. doi: 10.3390/ijms21083010 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Przewłócka, K., Folwarski, M., Kaźmierczak-Siedlecka, K., Skonieczna-Żydecka, K., and Kaczor, J. J. (2020). Gut-muscle axis exists and may affect skeletal muscle adaptation to training.Nutrients12:1451. doi: 10.3390/nu12051451 PubMed AbstractCrossRef Full TextGoogle Scholar .
The rising incidence of adult spinal deformities linked to sarcopenia highlights the need for further exploration into this fascinating gut-muscle interplay.
Gut Microbiota's Role in Spinal Degeneration Pain
Gut Microbiota (GM) plays a pivotal role in the symptoms of Spinal Degenerative Diseases (SDD), including low back pain and extremities' numbness or pain.
GM is involved in producing Short-Chain Fatty Acids (SCFA), neurotransmitters, and vitamins that significantly regulate inflammation and pain, thereby influencing SDD-derived pain A Trusted Source Barton, W., Penney, N. C., Cronin, O., Garcia-Perez, I., Molloy, M. G., Holmes, E., et al. (2018). The microbiome of professional athletes differs from that of more sedentary subjects in composition and particularly at the functional metabolic level.Gut67, 313627–313633. doi: 10.1136/gutjnl-2016-313627 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Lucas, S., Omata, Y., Hofmann, J., Böttcher, M., Iljazovic, A., Sarter, K., et al. (2018). Short-chain fatty acids regulate systemic bone mass and protect from pathological bone loss.Nat. Commun.9:55. doi: 10.1038/s41467-017-02490-4 CrossRef Full TextGoogle Scholar .
GM produces neurotransmitters, like dopamine, serotonin, and GABA, crucial in pain modulation and analgesia A Trusted Source Liu, J., Xu, F., Nie, Z., and Shao, L. (2020). Gut microbiota approach-a new strategy to treat Parkinson's disease.Front. Cell. Infect. Microbiol.10:570658. doi: 10.3389/fcimb.2020.570658 PubMed AbstractCrossRef Full TextGoogle Scholar .
B vitamins from GM also exhibit analgesic effects through their anti-inflammatory, antinociceptive, and neuroprotective properties A Trusted Source Buesing, S., Costa, M., Schilling, J. M., and Moeller-Bertram, T. (2019). Vitamin B12 as a treatment for pain.Pain Physician1, E45–E52. doi: 10.36076/ppj/2019.22.E45 PubMed AbstractCrossRef Full TextGoogle Scholar .
Moreover, an abnormal GM composition has been linked to various pain-related conditions like low back pain, fibromyalgia, chronic pain, and osteoarthritis, highlighting GM's potential role in individual pain sensitivity differences A Trusted Source Dekker Nitert, M., Mousa, A., Barrett, H. L., Naderpoor, N., and de Courten, B. (2020). Altered gut microbiota composition is associated with back pain in overweight and obese individuals.Front. Endocrinol.11:605. doi: 10.3389/fendo.2020.00605 PubMed AbstractCrossRef Full TextGoogle Scholar A Trusted Source Ellis, R. J., Heaton, R. K., Gianella, S., Rahman, G., and Knight, R. (2022). Reduced gut microbiome diversity in people with HIV who have distal neuropathic pain.J. Pain23, 318–325. doi: 10.1016/j.jpain.2021.08.006 PubMed AbstractCrossRef Full TextGoogle Scholar .
However, this association with SDD-related pain is yet to be validated.
Analgesics used for SDD pain must be approached cautiously, as GM significantly affects drug response and effectiveness A Trusted Source Vich Vila, A., Collij, V., Sanna, S., Sinha, T., Imhann, F., Bourgonje, A. R., et al. (2020). Impact of commonly used drugs on the composition and metabolic function of the gut microbiota.Nat. Commun.11:362. doi: 10.1038/s41467-019-14177-z PubMed AbstractCrossRef Full TextGoogle Scholar .

Particularly with long-term opioid use, GM composition may be adversely affected, predisposing individuals to opioid tolerance A Trusted Source Akbarali, H. I., and Dewey, W. L. (2017). The gut-brain interaction in opioid tolerance.Curr. Opin. Pharmacol.37, 126–130. doi: 10.1016/j.coph.2017.10.012 PubMed AbstractCrossRef Full TextGoogle Scholar .
Therefore, exploring the interaction between GM and SDD-derived pain is crucial for understanding SDD's pathogenesis and improving individual analgesic efficacy and prognosis.
Discussion
The interplay between various components and their impact on overall outcomes has been elucidated in the preceding sections.
A thorough examination of the data underscores the interconnectedness of each element, pointing to the intricate web of cause and effect that characterizes this topic.
While substantial research has been conducted, there remains a degree of ambiguity that warrants further investigation.
The present findings have potential implications that could revolutionize our understanding and approach.
However, it's crucial to consider the limitations inherent in any study.
It's also worth noting that while certain trends and correlations were identified, a direct causative relationship has yet to be established conclusively.
Peer-reviewed studies, large-scale research, and multidisciplinary collaboration could further validate these initial findings.
Conclusion
In light of the findings discussed it becomes evident that a holistic approach, factoring in all the interconnected components, is essential for a comprehensive understanding.
The significance of these connections can't be understated, as they present promising avenues for future interventions and strategies.
However, as with all scientific endeavors, it's imperative to tread with caution, ensuring that conclusions are drawn from solid evidence rather than mere correlations.
As the field advances and more data becomes available, there's hope that clarity will emerge, providing a definitive roadmap for future action.
Meanwhile, continued exploration and collaboration remain the need of the hour, ensuring that every avenue is pursued to its fullest potential.
Review date not set.
How we reviewed this article:
Latest on:





